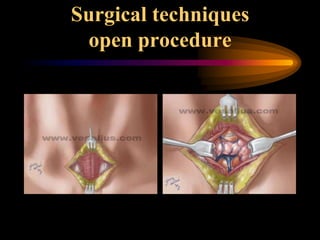
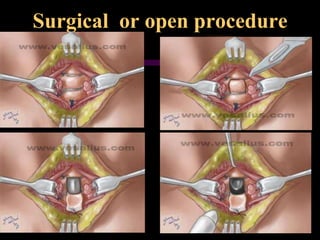
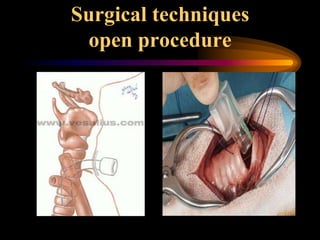
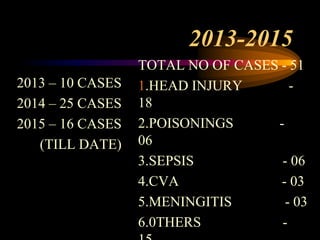
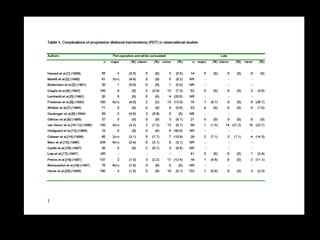
1. The document compares the surgical and percutaneous dilational tracheostomy (PCDT) procedures for creating a tracheostomy from 2013-2015.
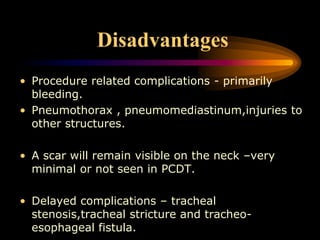
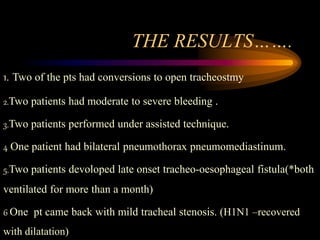
2. 51 total cases were performed, with 2 patients requiring conversion to an open procedure due to bleeding complications with PCDT.
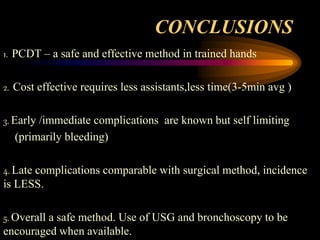
3. PCDT was found to be a safe and effective alternative to the open surgical procedure with comparable late complications but lower early bleeding risks and cost.