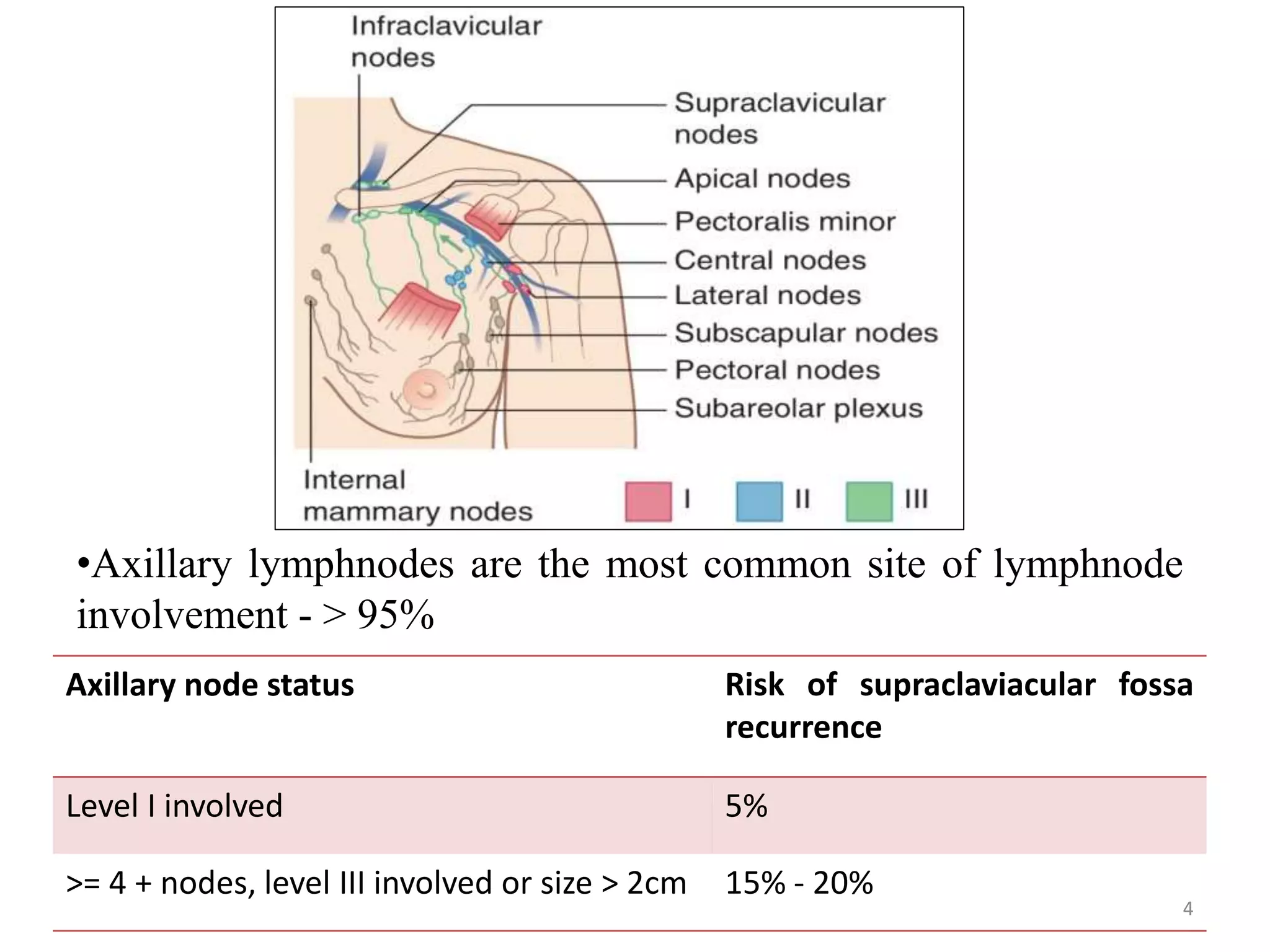
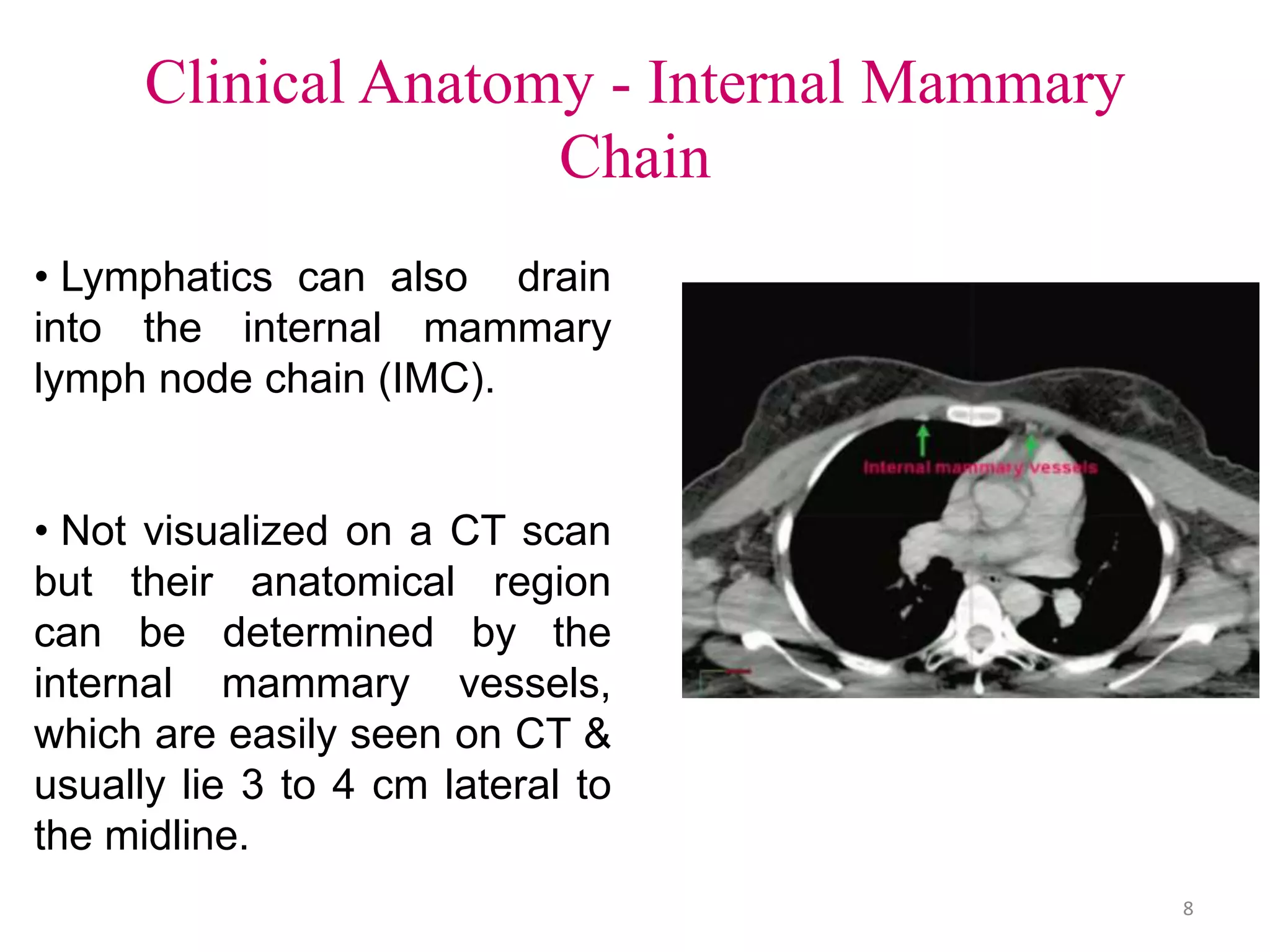
Regional lymph nodes, including the axillary, supraclavicular, and internal mammary nodes, are important sites of potential breast cancer spread. Axillary ultrasound and sentinel lymph node biopsy help assess lymph node status. Several landmark trials have evaluated the benefits of radiotherapy to regional lymph nodes. The EBCTCG meta-analysis found regional radiotherapy reduced recurrence and breast cancer mortality in patients with 1-3 or 4+ positive lymph nodes. Current guidelines recommend regional radiotherapy for patients with extensive lymph node involvement or other high-risk features.