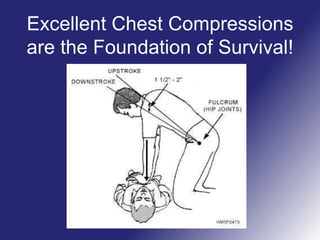
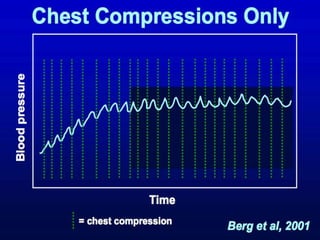
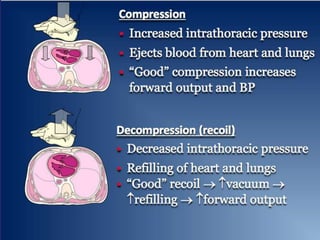
This document discusses the importance of effective chest compressions during cardiopulmonary resuscitation (CPR). It notes that recent American Heart Association guidelines have emphasized minimizing interruptions to chest compressions and limiting ventilation rates during CPR. The document explains that chest compressions are critical for increasing survival, especially when collapse to shock time is greater than 15 minutes. It also discusses how excessive or interrupted ventilations can decrease blood flow and notes that observed CPR often involves too many ventilations contrary to guidelines. The key message is that effective, continuous chest compressions with few interruptions and limited ventilations are the most important aspect of CPR.