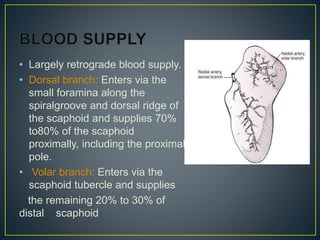
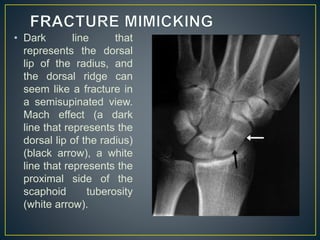
The scaphoid bone is located in the wrist and is vulnerable to injury due to its position. It has a tenuous blood supply and reduced healing capacity. Scaphoid fractures are difficult to diagnose on initial imaging and occur most commonly at the waist of the bone. Treatment depends on fracture pattern and stability, with nondisplaced fractures typically treated non-operatively with casting and displaced or unstable fractures often requiring surgical fixation. While casting results in immobilization, surgical treatment allows for earlier rehabilitation and return to activity.