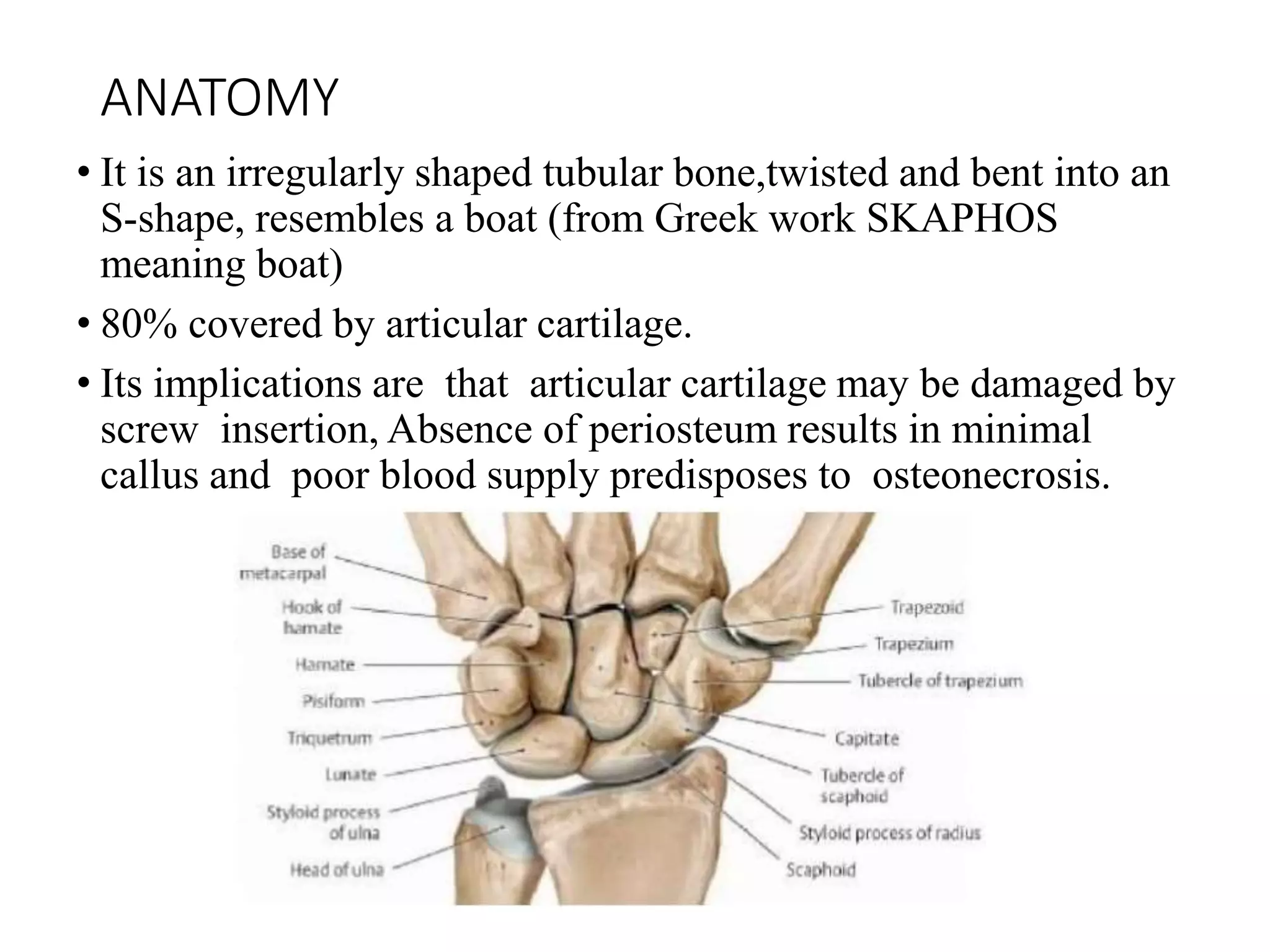
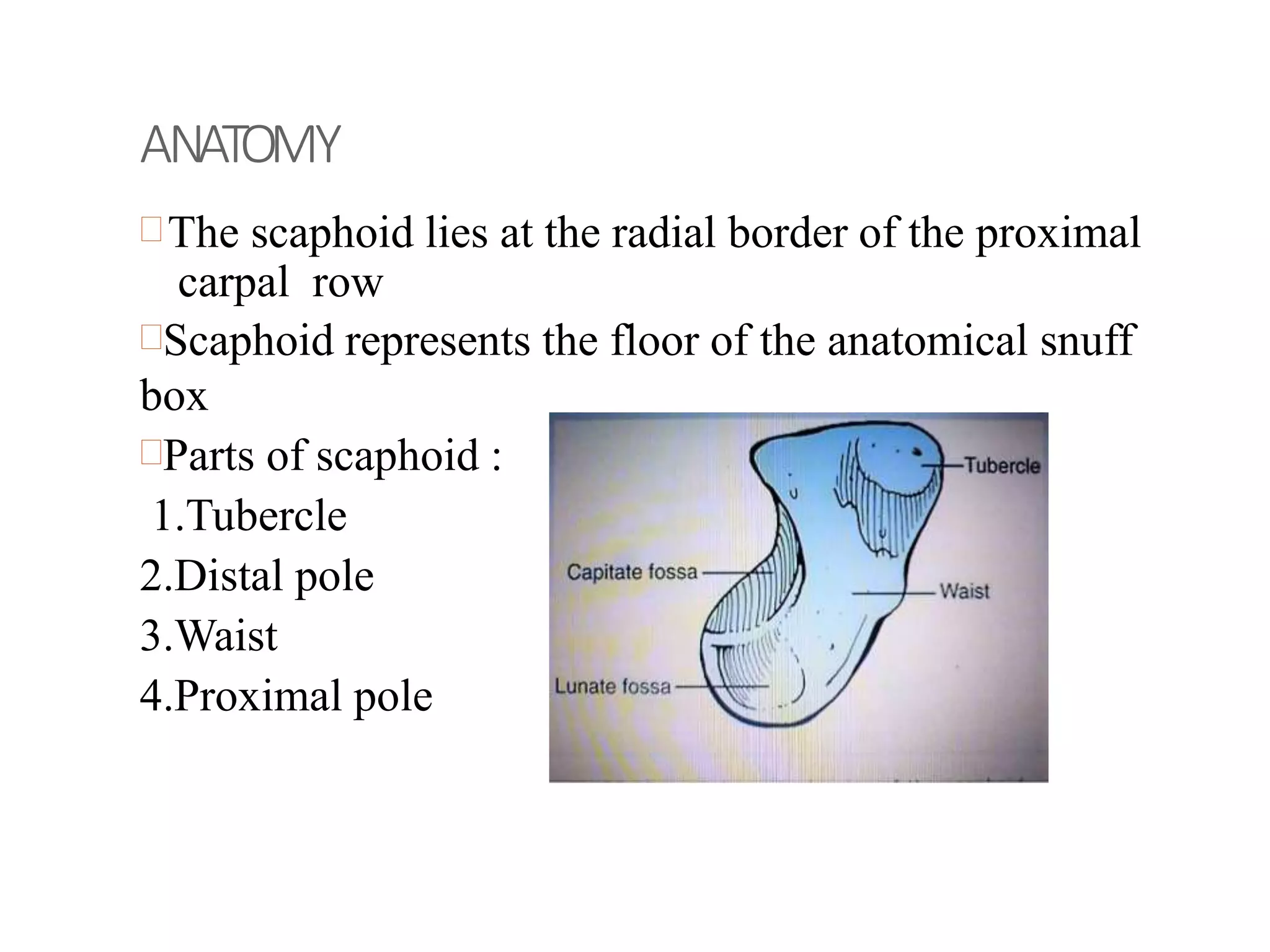
The document discusses scaphoid fractures, including:
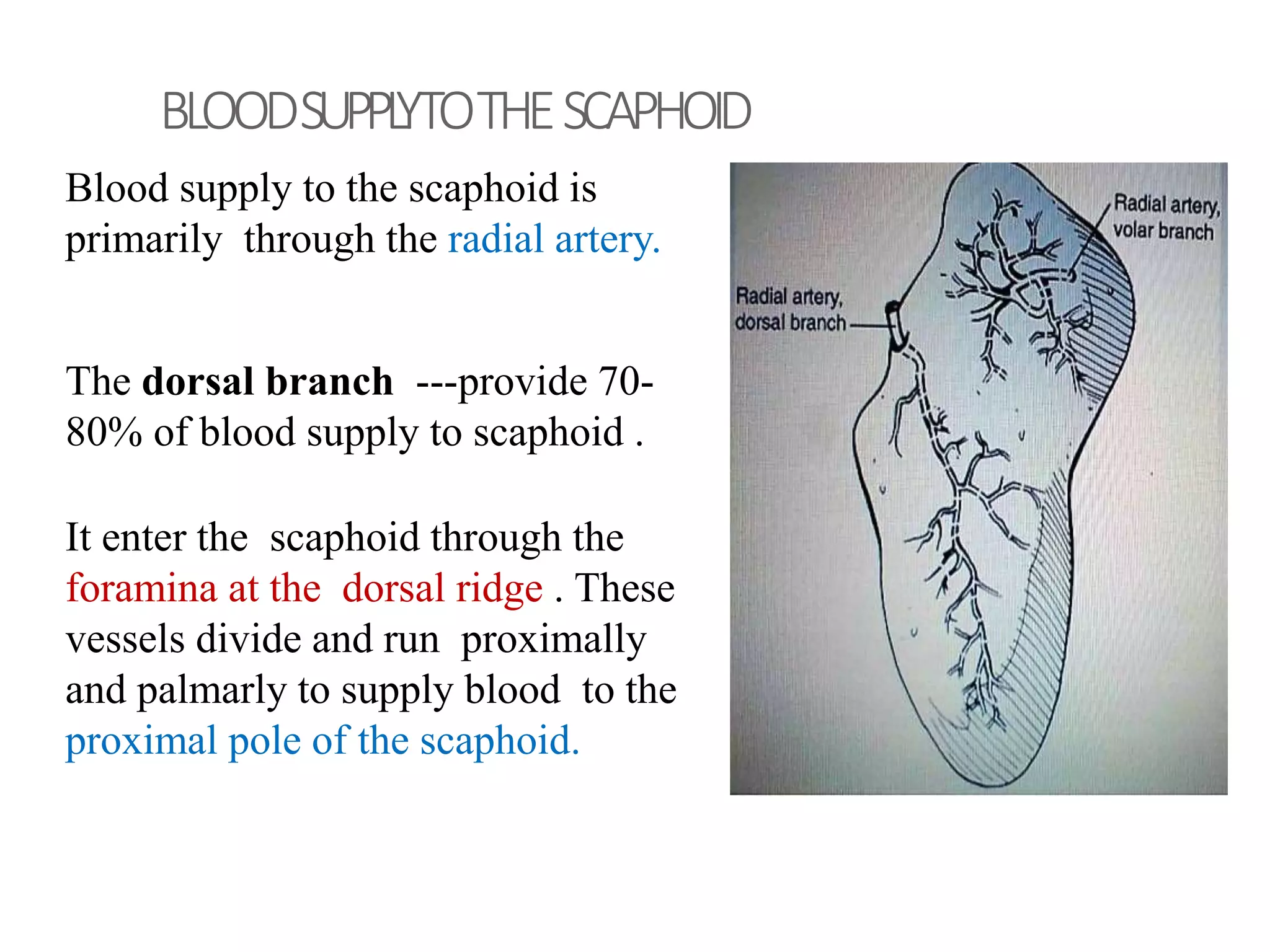
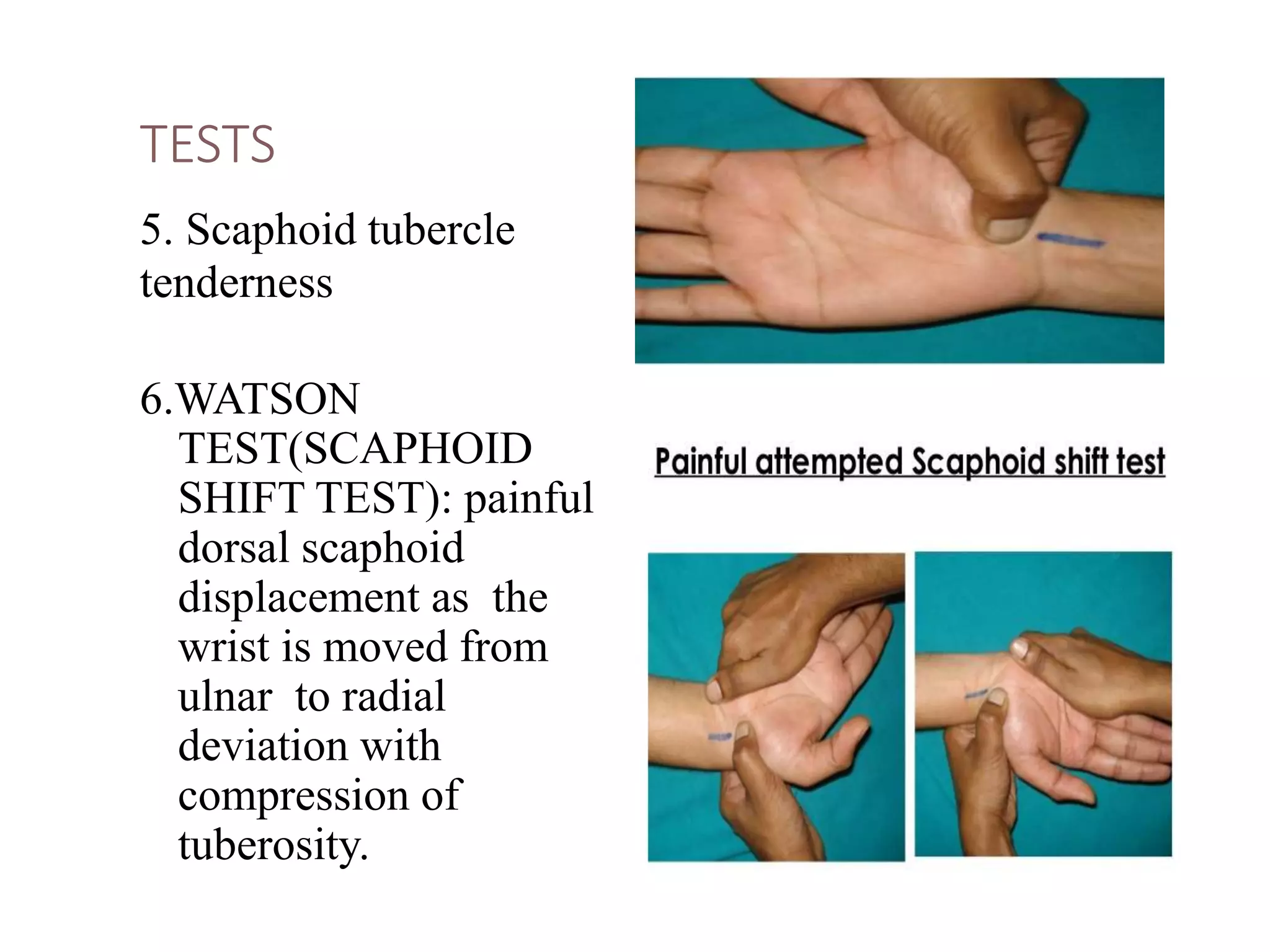
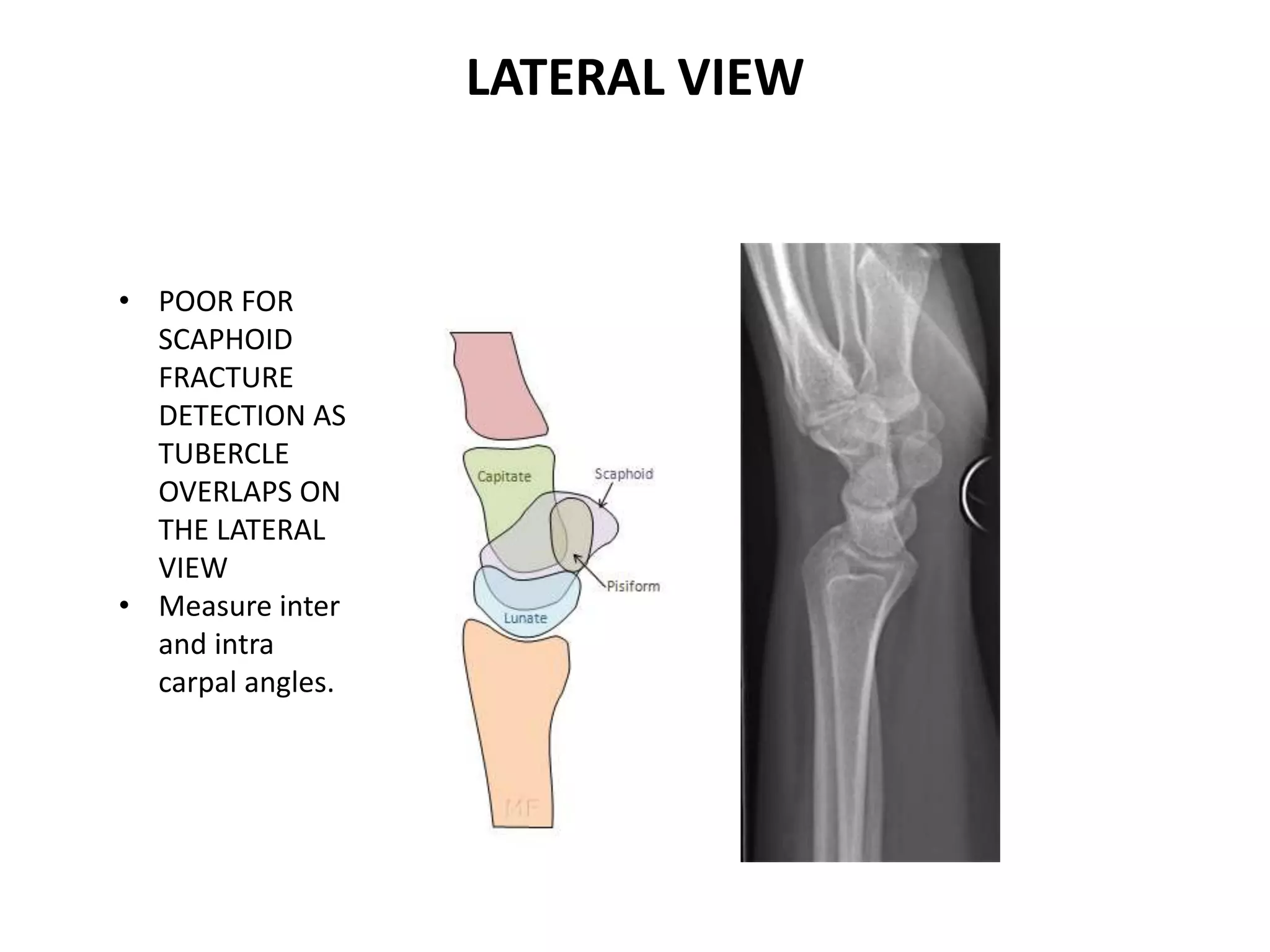
- Anatomy of the scaphoid bone and its blood supply.
- Mechanisms of injury typically involve falls on an outstretched hand causing hyperextension and radial deviation of the wrist.
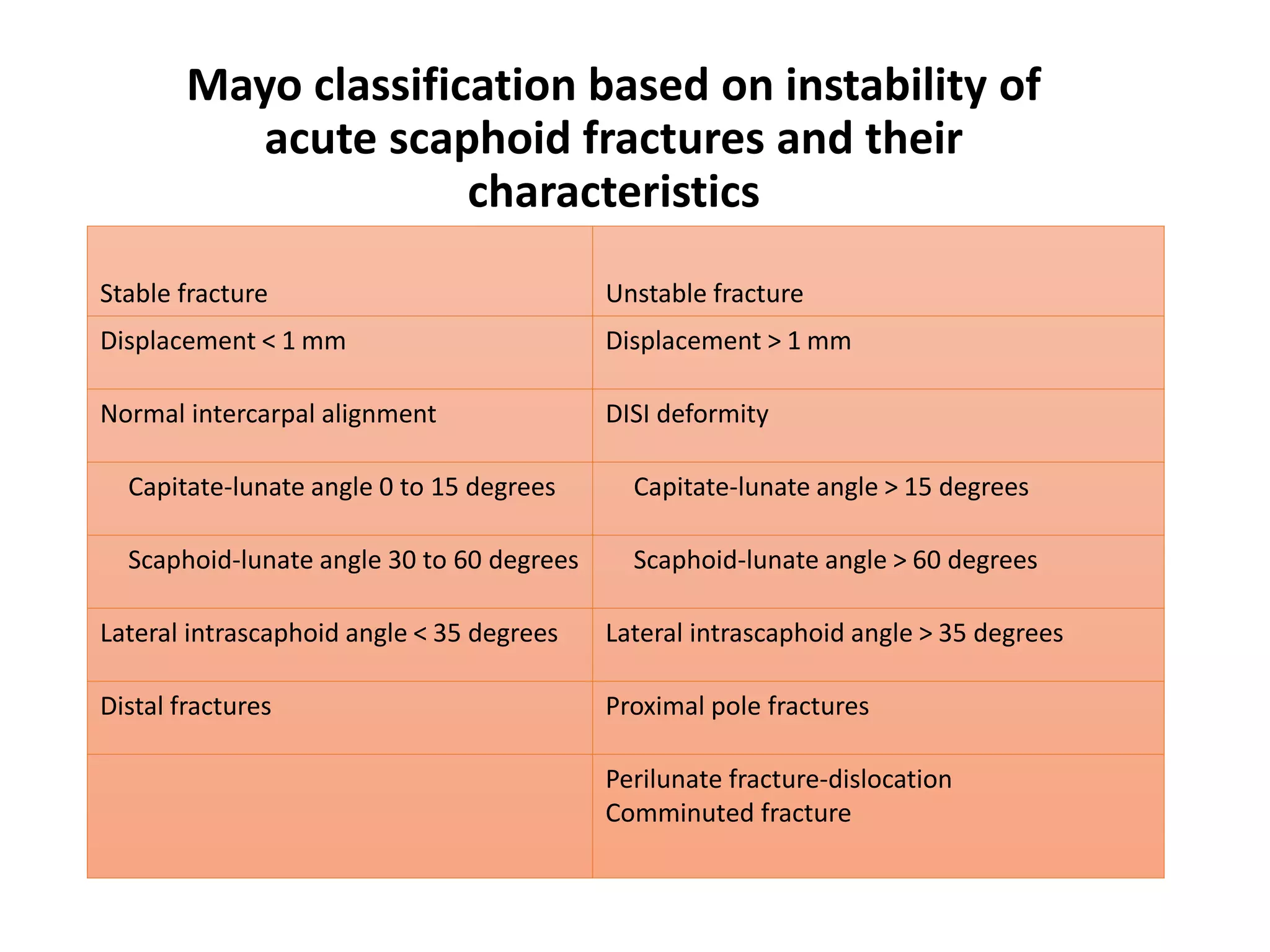
- Classification systems for scaphoid fractures include Russe's, Mayo, Herbert's, and AO.
- Treatment depends on fracture displacement and stability, ranging from cast immobilization for nondisplaced fractures to surgery for displaced or unstable fractures.

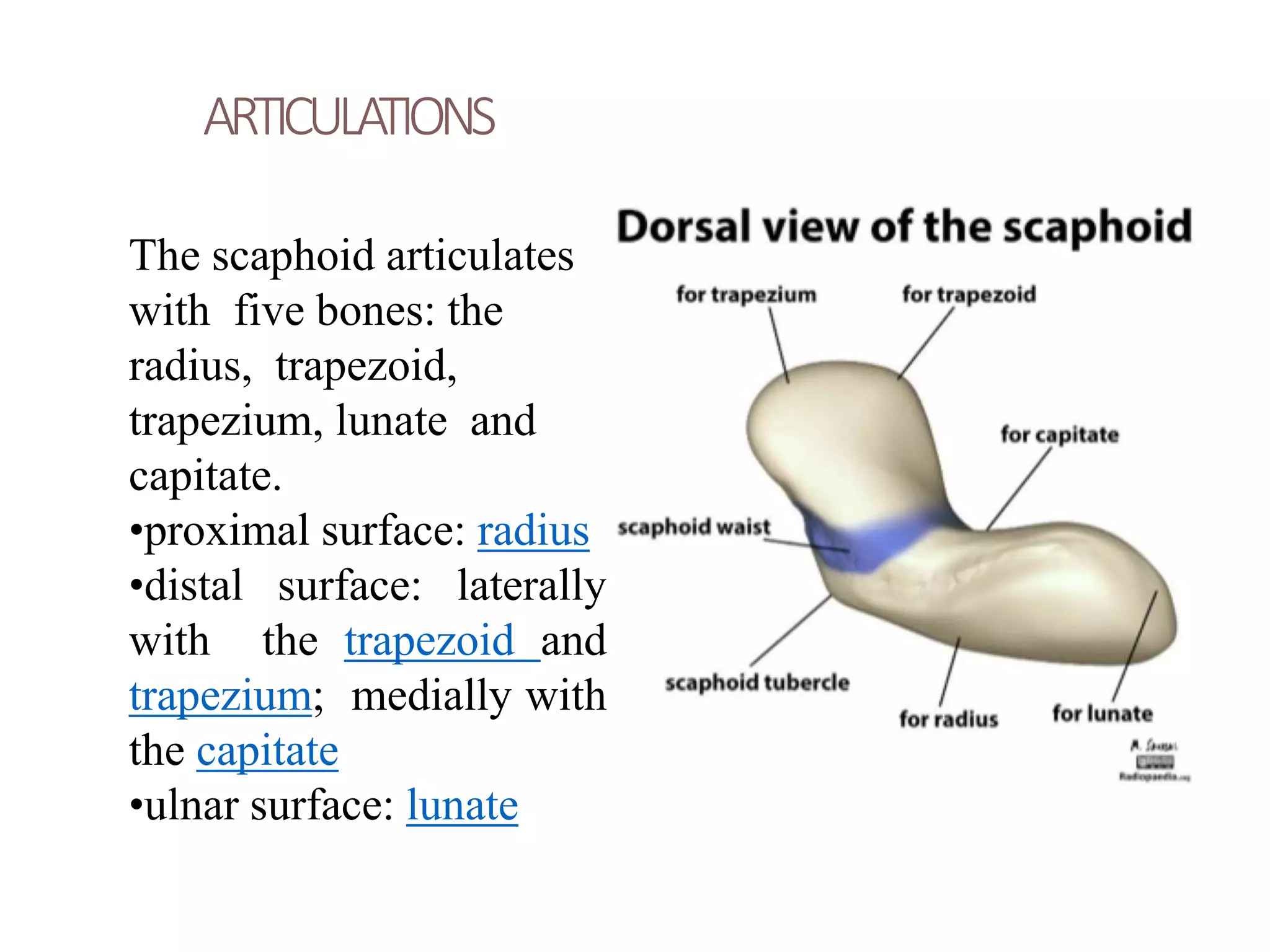



























































![SLADE AND GIESSLER
CLASSIFICATIONFORSCAPHOID
NONUNION
Type Iinjury : are the result ofadelayedpresentation (4 to 12
weeksafter injury).
TypeIIinjuries: afibrousunion is present.
TypeIIIinjuries: minimalsclerosisisseenat the fracture site.
Sclerosis< 1mm.
Type IVinjuries: cysticformation is present.
Type Vinjuries: cysticchanges> 5 mmin diameter, rotation of
the lunate hasoccurred, resulting in ahumpbackdeformityas
seenwith plainradiographyor CT.
TypeVIinjuries: secondarydegenerative changesare present,
(i.e., scaphoidnonunion advancedcollapse [SNAC]).](https://image.slidesharecdn.com/scaphoidfractureandnon-union-181204144602/75/Scaphoid-fracture-and-non-union-70-2048.jpg)



![KNOLL AND TRUMBLE ALGORITHM FOR MANAGEMENT OF
SCAPHOID NON UNION
(Adapted from Knoll VD, TrumbleTE:
Scaphoid fractures and nonunions, in Trumble TE [ed]: Hand Surgery
Update 3.Rosemont, IL:American Academy of OrthopaedicSurgeons,
2003, pp161-173.)](https://image.slidesharecdn.com/scaphoidfractureandnon-union-181204144602/75/Scaphoid-fracture-and-non-union-74-2048.jpg)


























