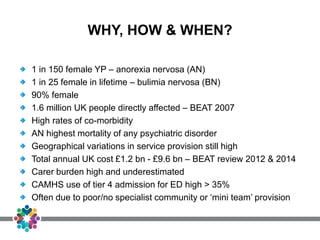
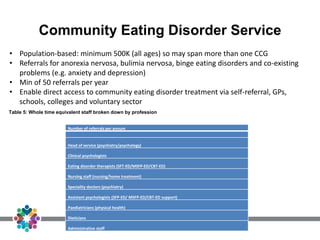
1. Eating disorders, especially anorexia nervosa, affect many young people in the UK, costing billions annually. Specialist community eating disorder services for children and youth (CEDS-CYP) are most effective but availability varies greatly.
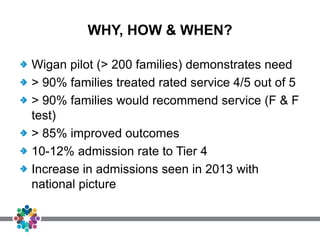
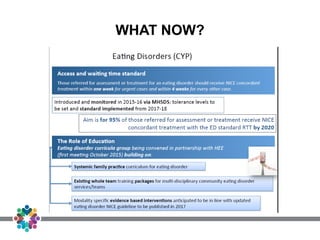
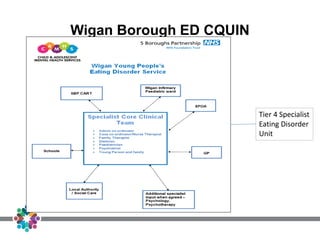
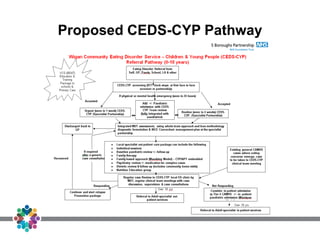
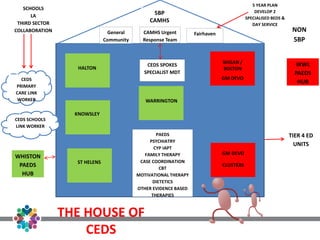
2. A pilot program in Wigan demonstrated the benefits of CEDS-CYP, with high family satisfaction and improved outcomes. Additional funding of £30 million over 5 years will support transforming eating disorder services in England for those under 18 through developing more CEDS-CYP teams.
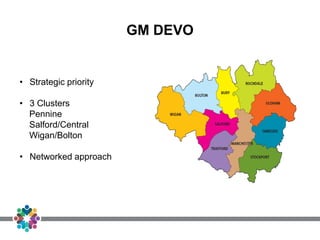
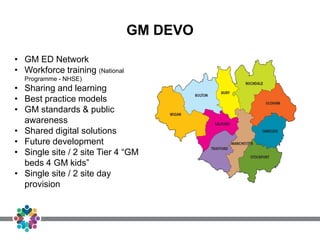
3. Greater Manchester aims to improve eating disorder care through a networked approach across clusters, developing workforce training, sharing best practices, and potentially consolidating tier 4 inpatient and