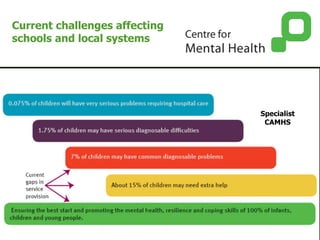
- Three children in every classroom have a diagnosable mental health difficulty, yet most do not receive help until much later in life. Early intervention can improve outcomes.
- Perinatal mental illness is a major risk factor for children's mental health, but only half of mothers are identified and receive treatment despite regular contact with primary care. Integration of perinatal services is important.
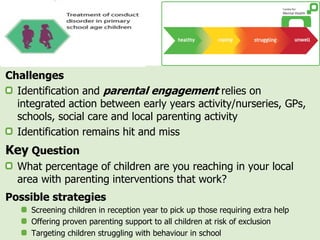
- Conduct problems are very common in children but often go unidentified and untreated. Parenting interventions can be effective but often do not reach enough families. Increased screening and support is needed.
- Schools play a key role in children's mental health but often lack guidance on local support services and resources to promote wellbeing. Increased partnerships between