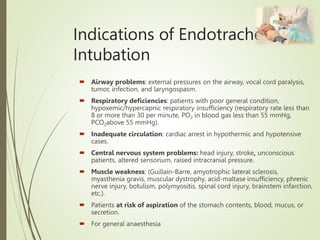
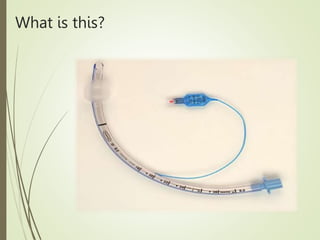
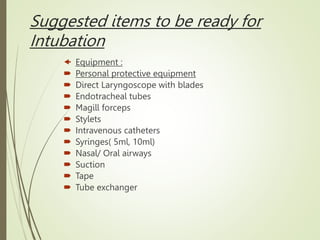
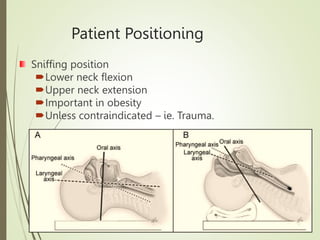
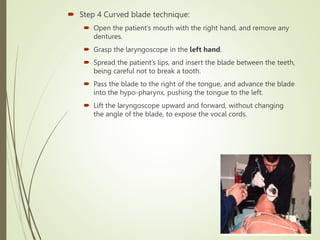
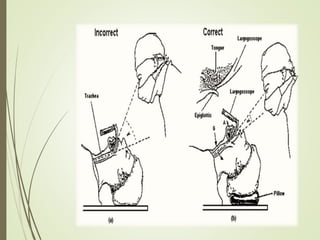
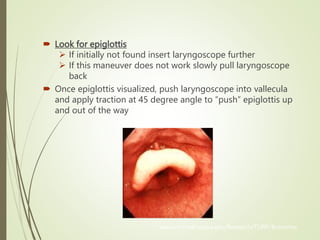
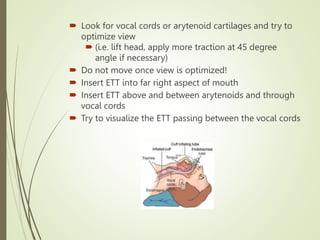
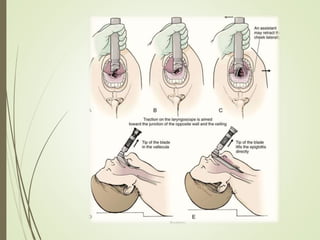
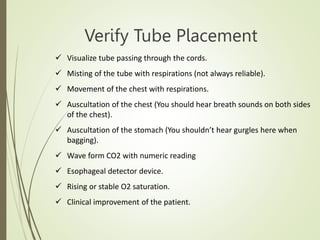
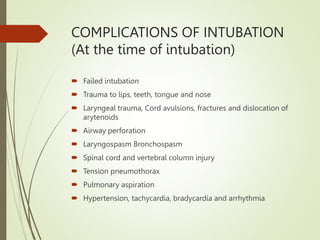
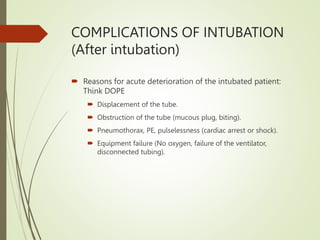
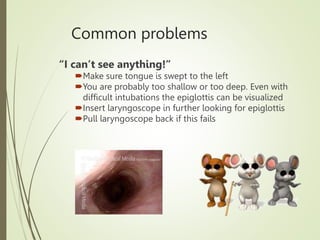
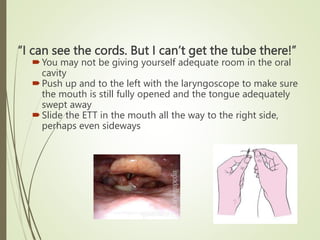
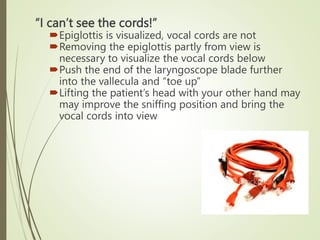
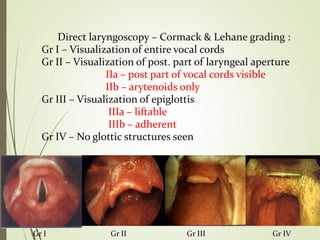
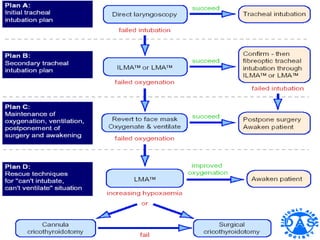
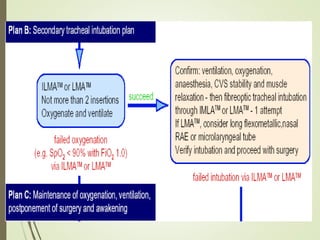
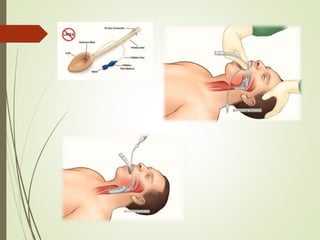
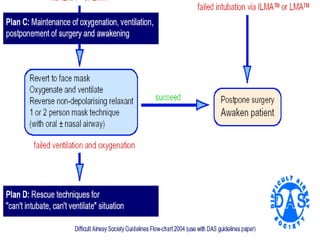
Endotracheal intubation is used to secure an airway in patients with airway issues, respiratory deficiencies, circulatory problems, neurological issues, or muscle weakness. The document outlines the proper procedure for intubating a patient including positioning them in sniffing position, using a curved blade laryngoscope to visualize the vocal cords, and carefully sliding the endotracheal tube between the cords. Placement must be verified and potential complications addressed. Difficult intubations may require alternate techniques if the cords cannot be initially seen such as pushing the laryngoscope further in or adjusting the patient's head position.