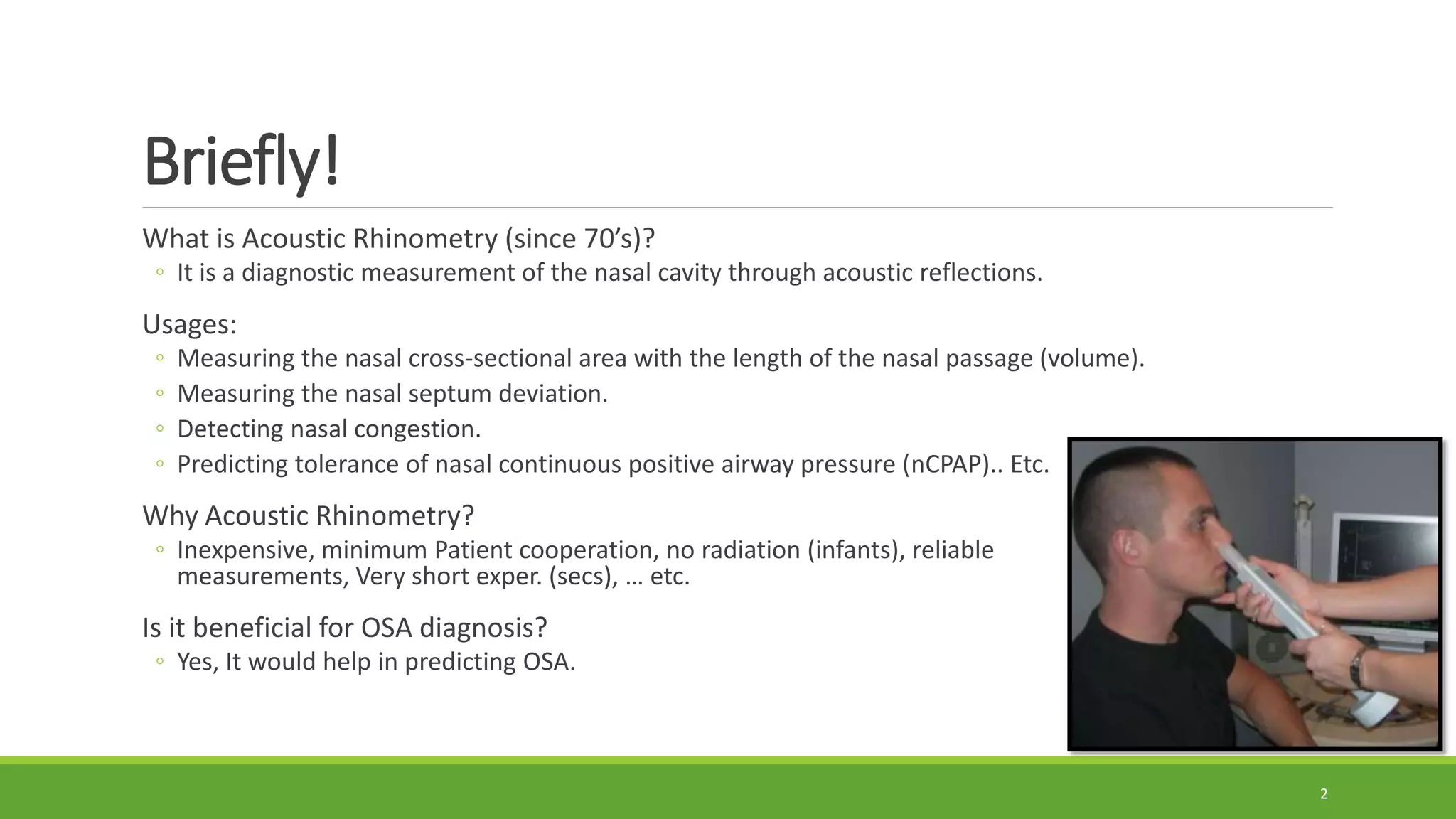
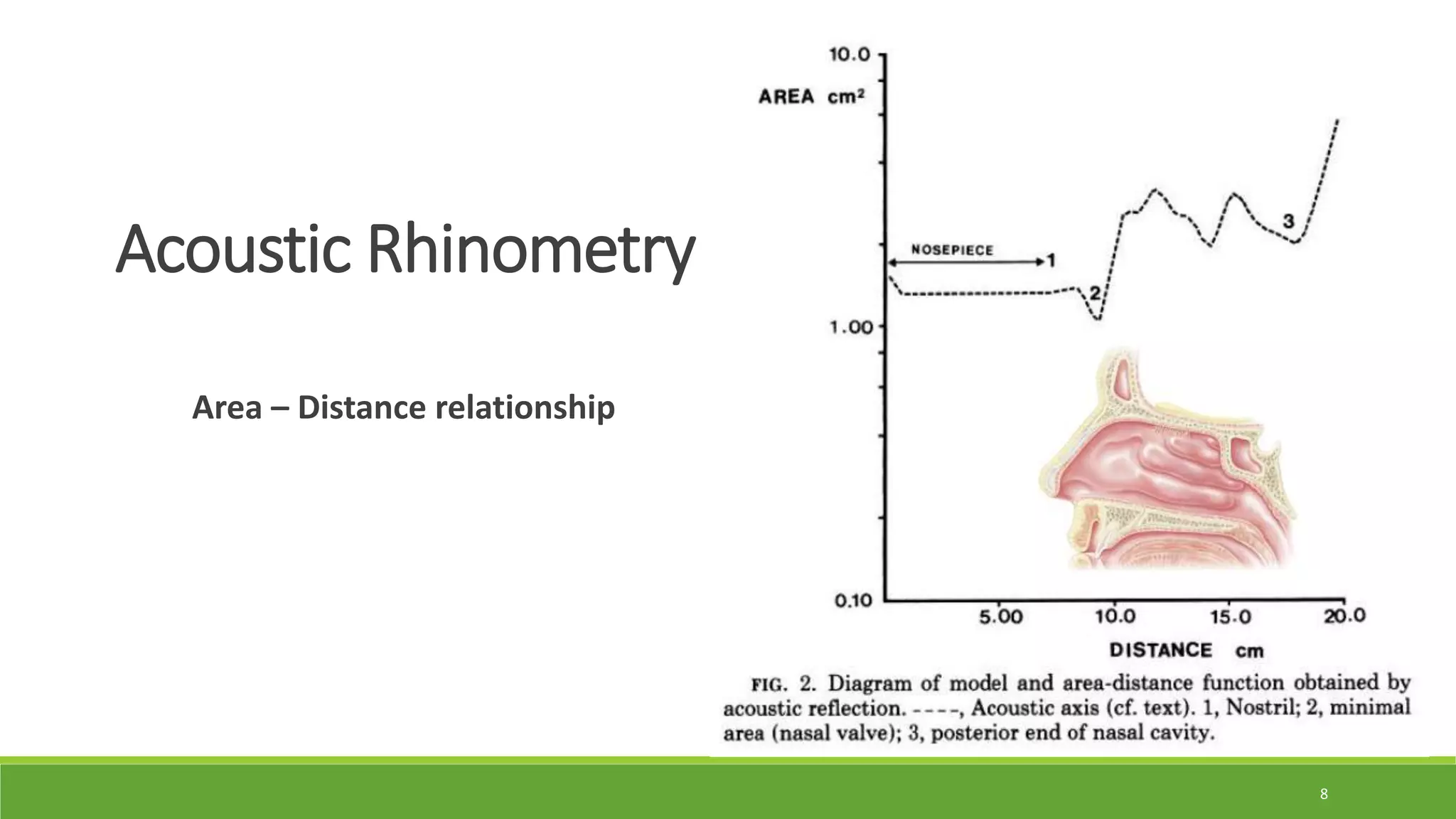
Acoustic rhinometry uses sound waves to non-invasively measure the nasal cavity geometry. It can detect nasal obstruction, septal deviations, and changes in nasal patency from congestion. A study found greater nasal congestion in patients with mild sleep apnea compared to non-apnea patients with allergic rhinitis, as measured by acoustic rhinometry before and after decongestion. This suggests nasal obstruction from rhinitis may contribute to the development of sleep apnea. Acoustic rhinometry provides a reliable, non-invasive way to investigate the nasal cavity and its role in sleep apnea.
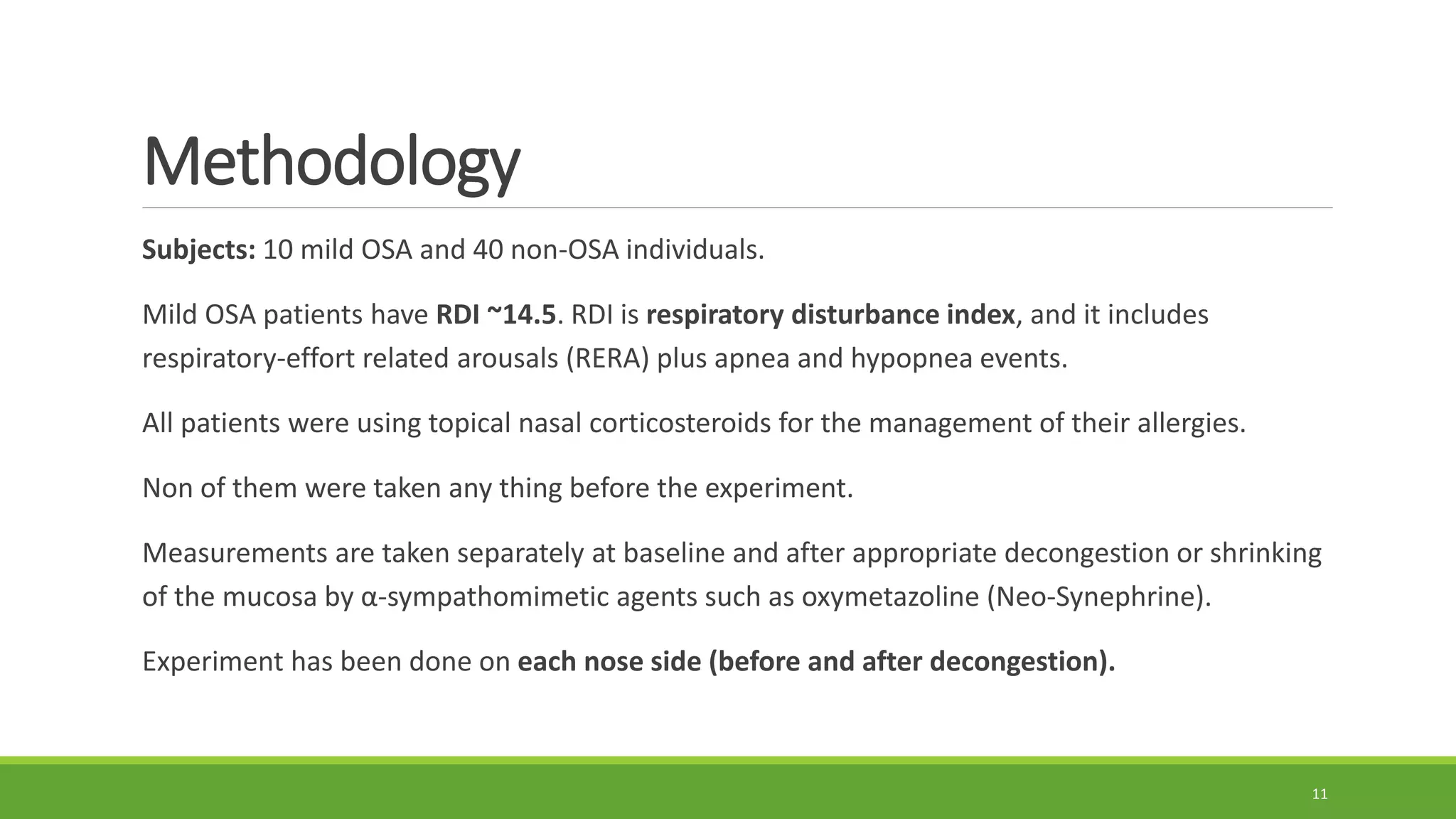
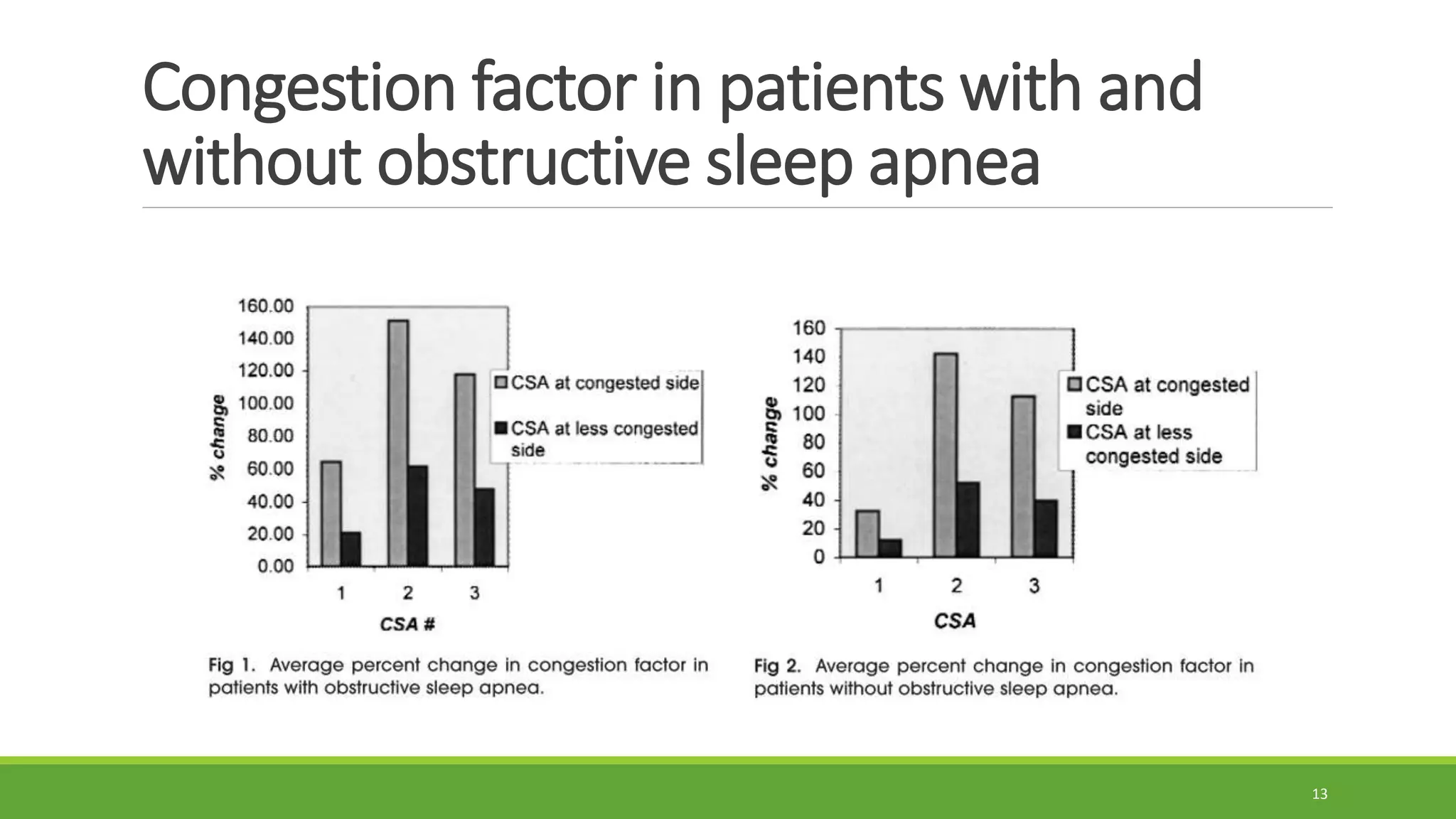
![Used parameters
CSA1 (~2 cm) the anterior portion of the inferior turbinate
CSA2 (~4 cm) the anterior portion of the middle turbinate
CSA3 (~6 cm) the middle portion of the middle turbinate
Congestion factor (%) = [(congested – decongested)CSA] x 100
12](https://image.slidesharecdn.com/rhinometrypresentation-180622223554/75/Rhinometry-presentation-12-2048.jpg)