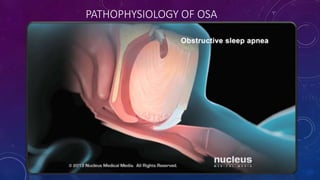
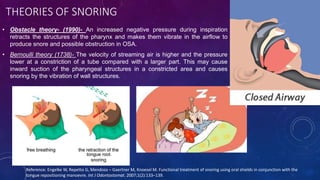
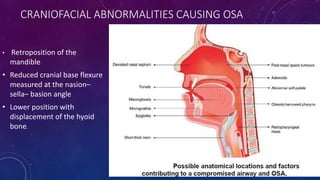
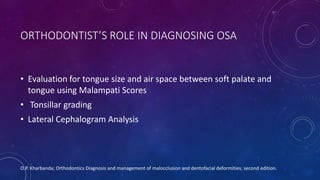
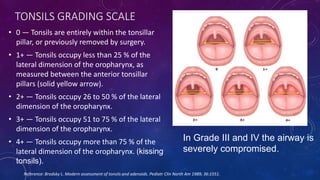
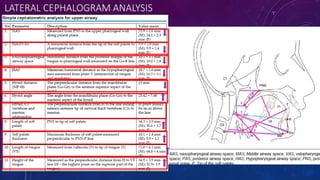
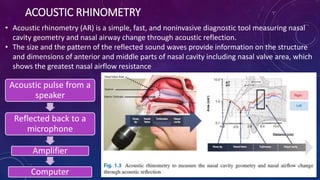
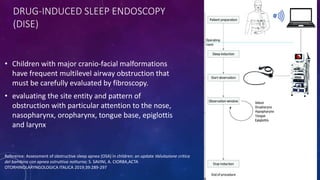
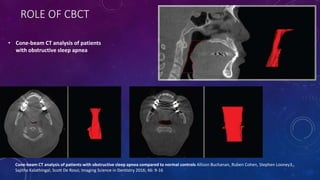
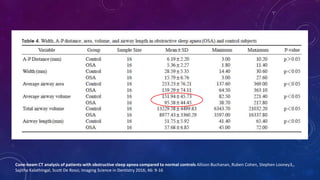
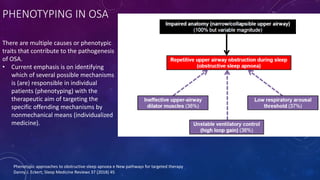
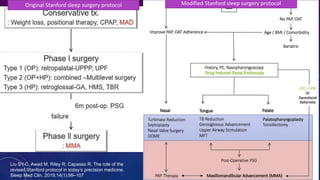
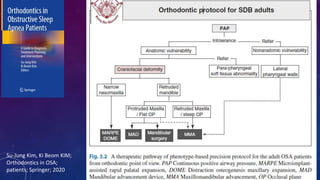
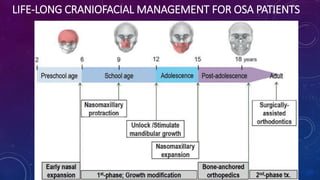
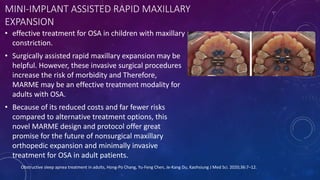
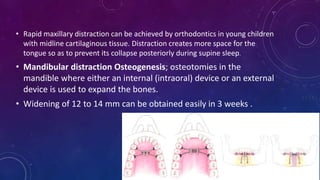
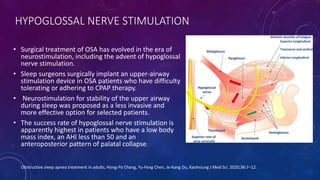
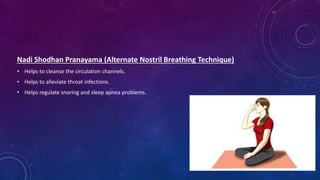
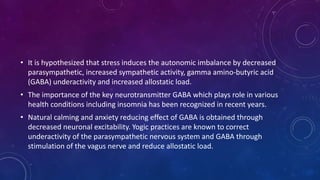
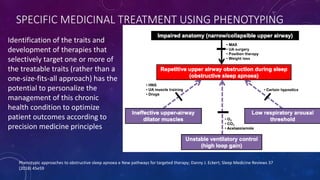
This document provides an overview of obstructive sleep apnea (OSA), including its diagnosis and treatment. It discusses the orthodontist's role in diagnosing OSA using tools like Mallampati scoring and lateral cephalograms. Treatment options covered include rapid maxillary expansion, distraction osteogenesis, hypoglossal nerve stimulation, and pranayama breathing exercises. The document concludes that a multidisciplinary approach including orthodontic, orthopedic, and surgical craniofacial treatments throughout life can effectively manage sleep-disordered breathing with craniofacial risk factors.