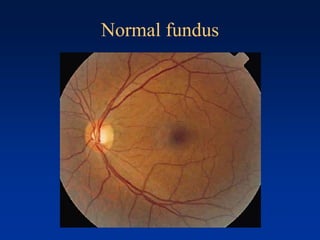
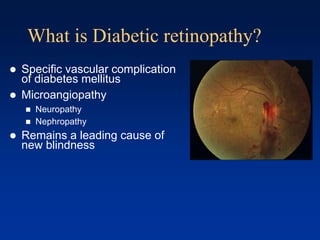
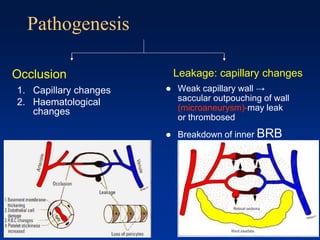
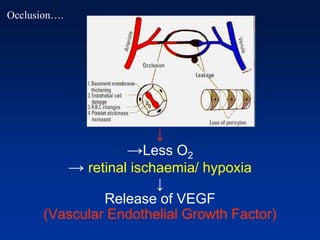
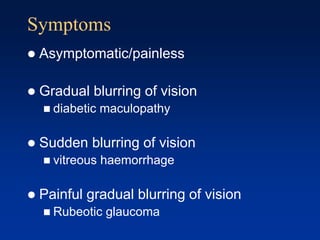
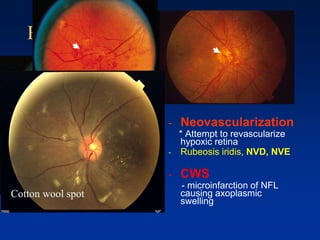
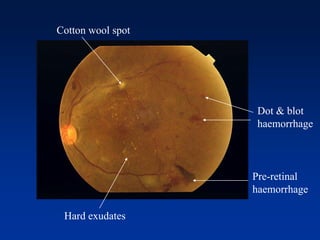
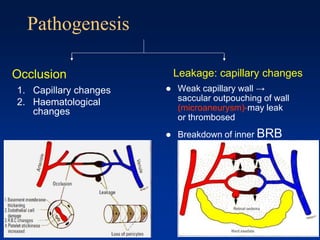
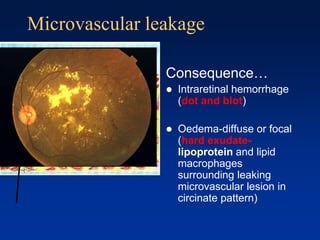
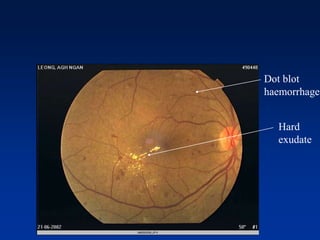
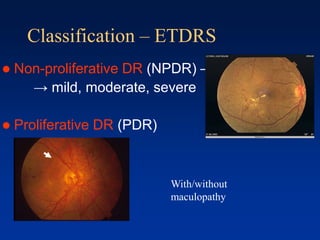
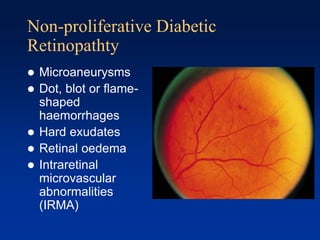
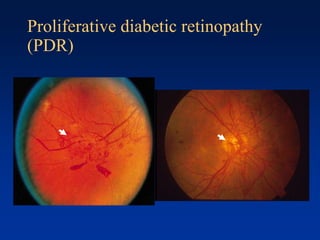
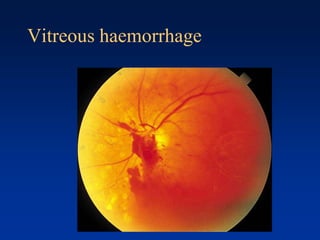
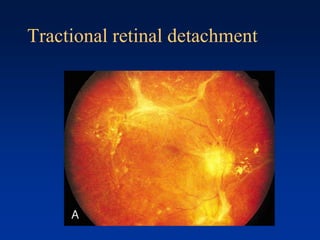
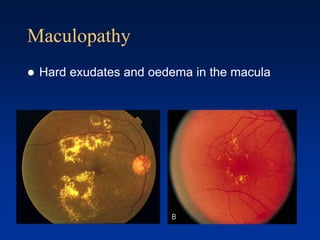
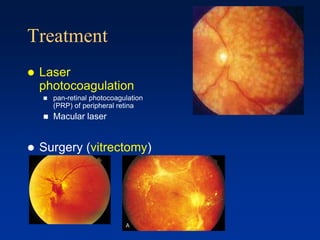
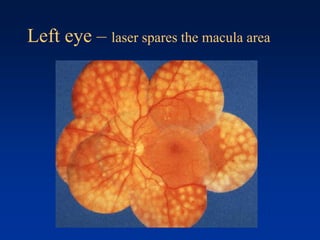
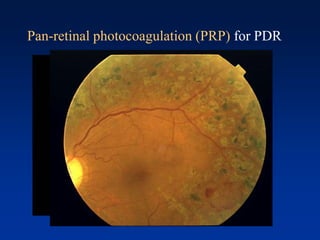
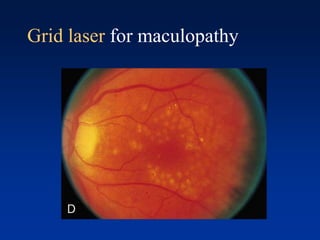
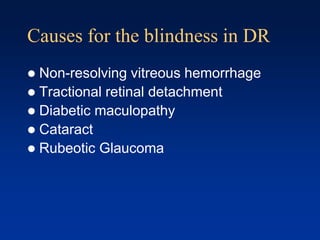
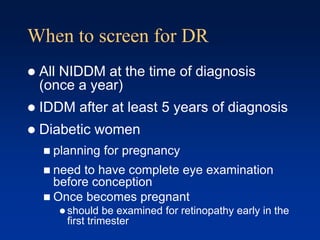
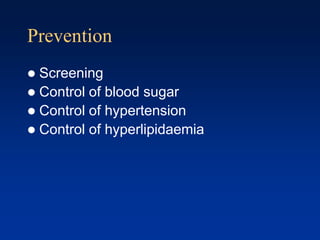
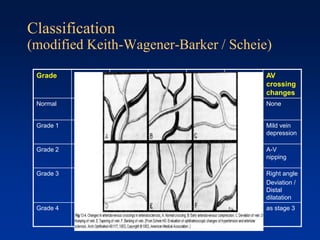
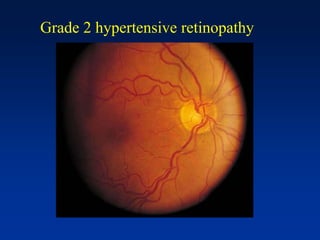
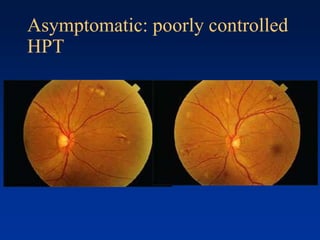
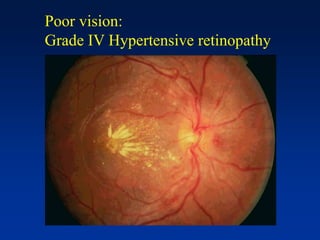
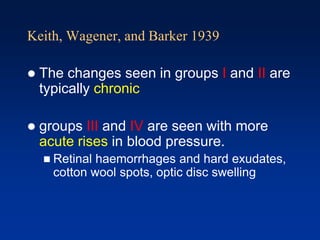
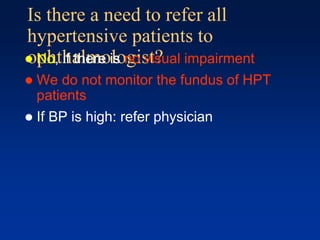
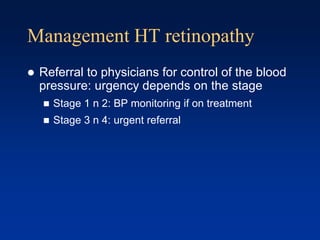
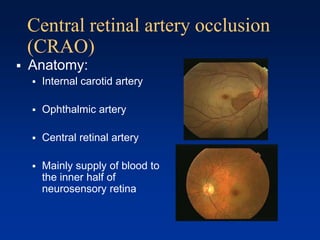
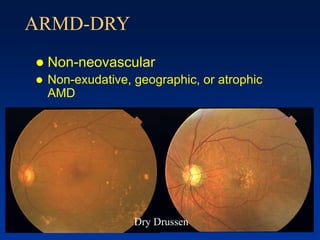
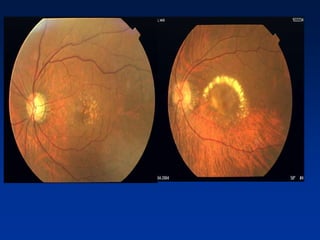
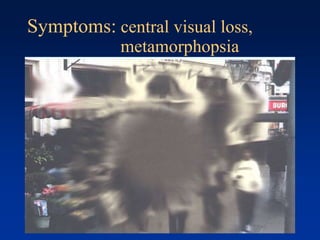
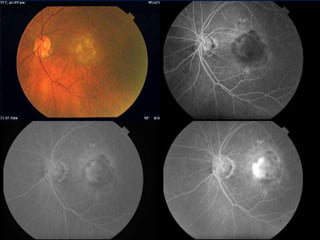
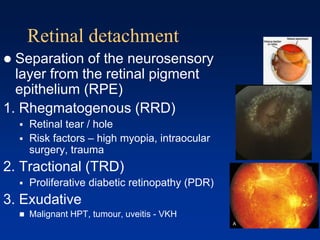
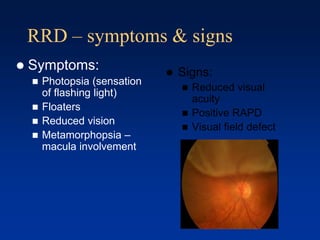
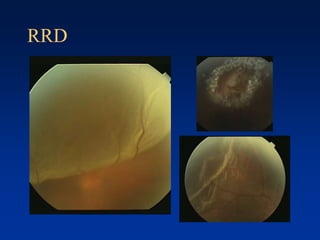
This document provides an overview of common retinal diseases, including diabetes mellitus, hypertension, retinal vascular disorders, age-related macular degeneration, and retinal detachment. It describes the pathogenesis, symptoms, classifications, and treatments for each condition. For diabetes mellitus, it discusses diabetic retinopathy in detail, from microaneurysms and neovascularization to laser treatment options. For hypertension, it covers hypertensive changes to the retina and their grading system. Age-related macular degeneration is differentiated as dry or wet forms. Retinal detachment causes and management are also outlined.