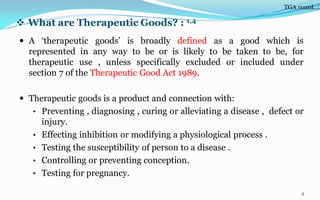
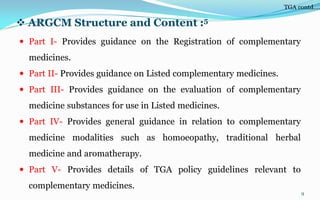
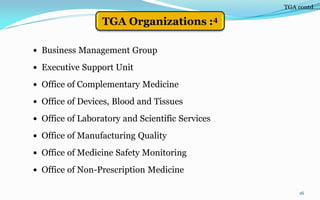
The Therapeutic Goods Administration (TGA) is the regulatory body for therapeutic goods in Australia. The TGA ensures medicines and medical devices available in Australia are safe and effective by conducting pre-market assessment and post-market surveillance. It maintains the Australian Register of Therapeutic Goods which lists all approved therapeutic goods. The TGA regulates medicines and medical devices according to risk level and oversees manufacturing licensing and good practices.