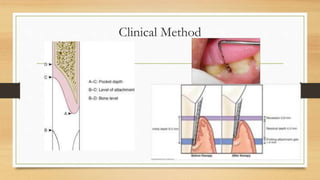
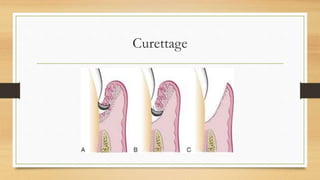
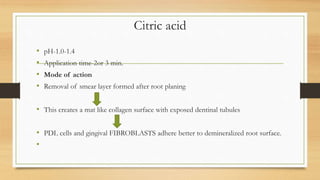
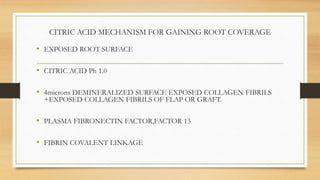
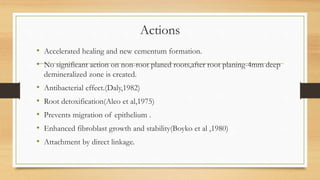
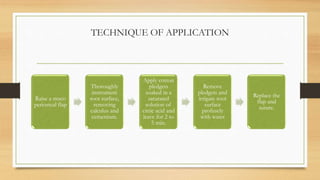
The document outlines various techniques and materials for reconstructive periodontal surgery, focusing on methods for enhancing periodontal attachment and healing. It discusses the roles of biologic mediators, grafting materials, and non-bone substitutes in treatments, as well as new attachment techniques that utilize citric acid and other agents to promote healing. Additionally, it provides clinical guidelines for selecting treatment protocols based on defect characteristics.



![Enamel Matrix Protein
• Amlogenin- secreted by HERS – tooth development—Acellular Cementum
formation– favor periodontal regeneration.
• Emdogain – marketed product [FDA approved]
Price $. 075.113.
0.3ml](https://image.slidesharecdn.com/reconstructiveperiodontalsurgery-161005144544/85/Reconstructive-periodontal-surgery-25-320.jpg)
![Technique
• Raised flap
• Debridement , control bleeding in defect
• Root surface treatment –citric acid or 24% EDTA(pH-6.7), 15 sec
• Rinse with saline
• Apply gel
• avoid contamination of wound by saliva and blood
• suture
• Systemic antibiotic[ doxycycline 100 mg ] for 10 to 21 days recommended
v](https://image.slidesharecdn.com/reconstructiveperiodontalsurgery-161005144544/85/Reconstructive-periodontal-surgery-27-320.jpg)
![• FDBA--- Osteoconductive
• DFDBA– Osteoinductive
• DFDBA more osteogenic---so preferable
• DFDBA—Demineralisation—in cold, diluted HCL acid
• Exposes –component of bone matrix---BMPs[bone morphogenetic protein]
• Cancellous DFDBA>>>Cortical DFDBA
• Osteogenin or BMP3 –bone inductive protein isolated from the extracellular
matrix of human bone—tested and found to enhance osseous regeneration.](https://image.slidesharecdn.com/reconstructiveperiodontalsurgery-161005144544/85/Reconstructive-periodontal-surgery-40-320.jpg)
![• Cartilage: serves as a scaffolding, received limited evaluation
• Plaster of Paris [calcium sulfate] : biocompatible, porous, allowing fluid
exchange, resorbs completely in 1 to 2 weeks.
• Usefulness in human studies not proved
• Plastic material : composite of Polymethyl-methacrylate and
Polyhydroxyethylmethacrylate.](https://image.slidesharecdn.com/reconstructiveperiodontalsurgery-161005144544/85/Reconstructive-periodontal-surgery-46-320.jpg)
![Coral Derived Material
• Two types:
• Natural coral [resorbed slowly-several months]
• Coral derived porous hydroxyapatite [ years for resorption]
• Shows microscopic cementum and bone formation
• But slow resorbability —limited clinical success](https://image.slidesharecdn.com/reconstructiveperiodontalsurgery-161005144544/85/Reconstructive-periodontal-surgery-49-320.jpg)
![Clinical Decision Tree
• For Deep, Well-Contained Defects—EMD alone, CAF (if necessary)
• For Moderate-Deep, Noncontained defects- EMD+Graft, CAF(if necessary)
• For Supracrestal Defects with a shallow Vertical Defect-
EMD+Graft+Barrier membrane, with Coronally Advanced Flap
EMD- enamel matrix derivative. Emdogain
[Froum et al 2001]](https://image.slidesharecdn.com/reconstructiveperiodontalsurgery-161005144544/85/Reconstructive-periodontal-surgery-51-320.jpg)