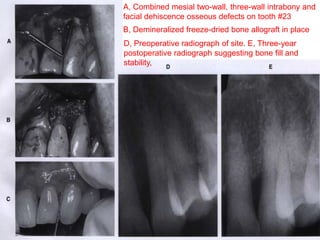
This document discusses reconstructive periodontal surgery techniques for regenerating lost periodontal structures, including regeneration and new attachment. It describes non-graft and graft-associated techniques using various bone graft materials such as autogenous, allograft, xenograft, and alloplastic grafts. Membranes are also discussed for use in guided tissue regeneration to prevent epithelial migration and promote new attachment from bone and periodontal ligament cells.