The document discusses advanced periodontal regeneration techniques, highlighting challenges in assessing periodontal wound healing and types of healing determined through histological studies. It outlines various reconstructive surgical techniques, the principles of osseous regeneration, and the evaluation methods for periodontal reconstruction, including clinical and radiographic assessments. Additionally, it covers graft classifications, root biomodification techniques, and the use of growth factors and enamel matrix proteins in promoting periodontal regeneration.
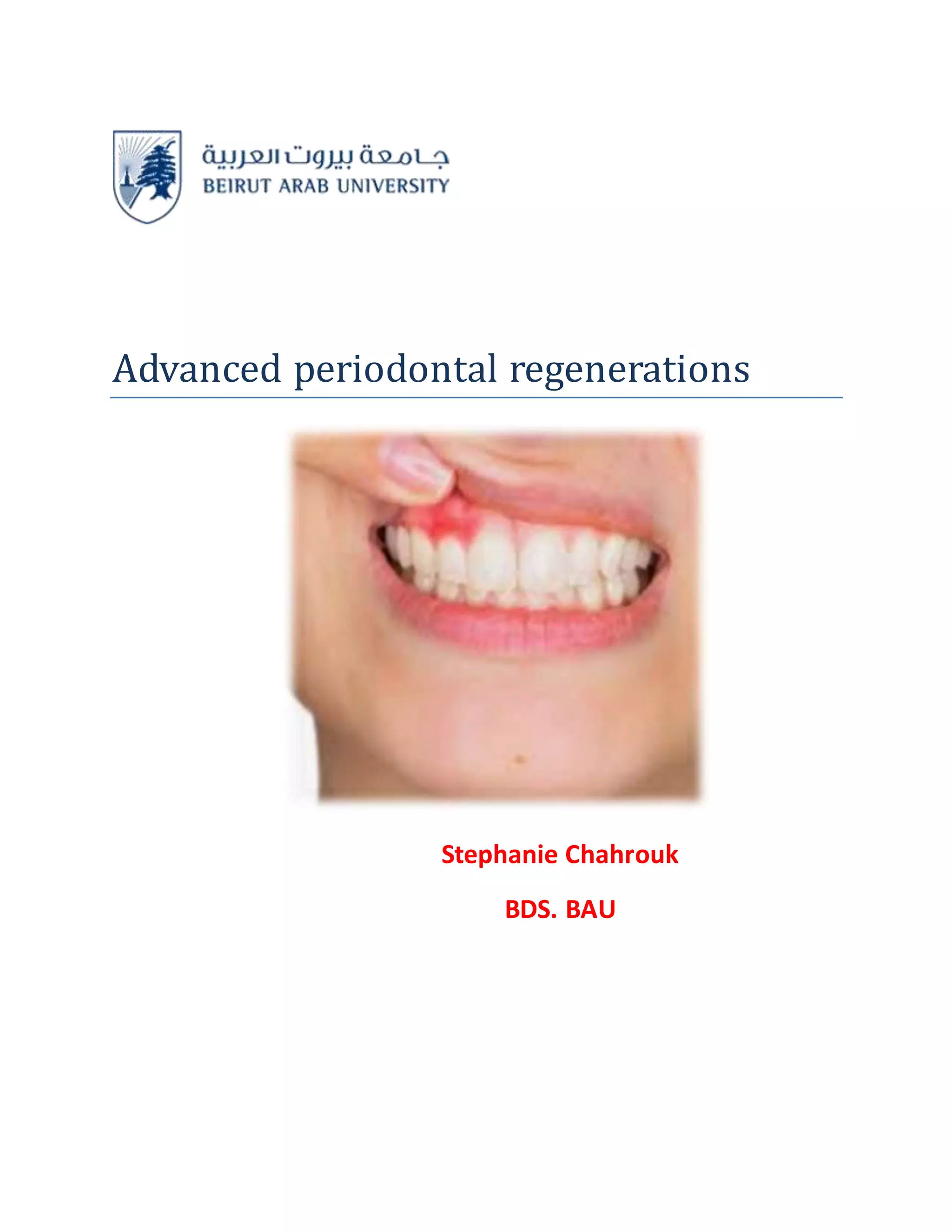











![“”Allograft and Xenograft”
1. “Foreign to body---risk to provoke immune response
2. Suppress antigenic potential—by radiation, freezing, chemical treatment
3. Allograft –DFDBA(Decalcified Freeze-Dried Bone Allograft ), FDBA
4. Commercially obtained—cortical bone—12 hours—death of DONOR ---Defatted----cut in
pieces---washed in absolute alcohol---deep frozen
5. May be demineralized then---ground and sieved---250 to 750um and
6. Freeze-dried
7. Finally Vacuum sealed in glass vials”
“FDBA--- Osteoconductive
DFDBA– Osteoinductive
DFDBA more osteogenic---so preferable
DFDBA—Demineralisation—in cold, diluted HCL acid
Exposes –component of bone matrix---BMPs[bone morphogenetic protein]
Cancellous DFDBA>>>Cortical DFDBA”
“Osteogenin or BMP3 –bone inductive protein isolated from the
extracellular matrix of human bone—tested and found to enhance osseous
regeneration.”
“Xenograft”
“• Calf bone [ Boplant –treated by detergent extraction—sterilized—freeze-dried.
• Kiel bone is calf or OX bone –denatured with 20% H2O2---Dries with Acetone—
Sterilized with ethylene oxide.
• Anorganic bone is OX bone—organic material extracted by---ethylenediamine--- then
sterilized by autoclaving.
• Ospurane : cow bone soaked in KOH , acetone and salt solution
• Boiled Bone: cow bone boiled or autoclaved”](https://image.slidesharecdn.com/perioassigmnt-190516132736/75/Advanced-periodontal-regenerations-21-2048.jpg)
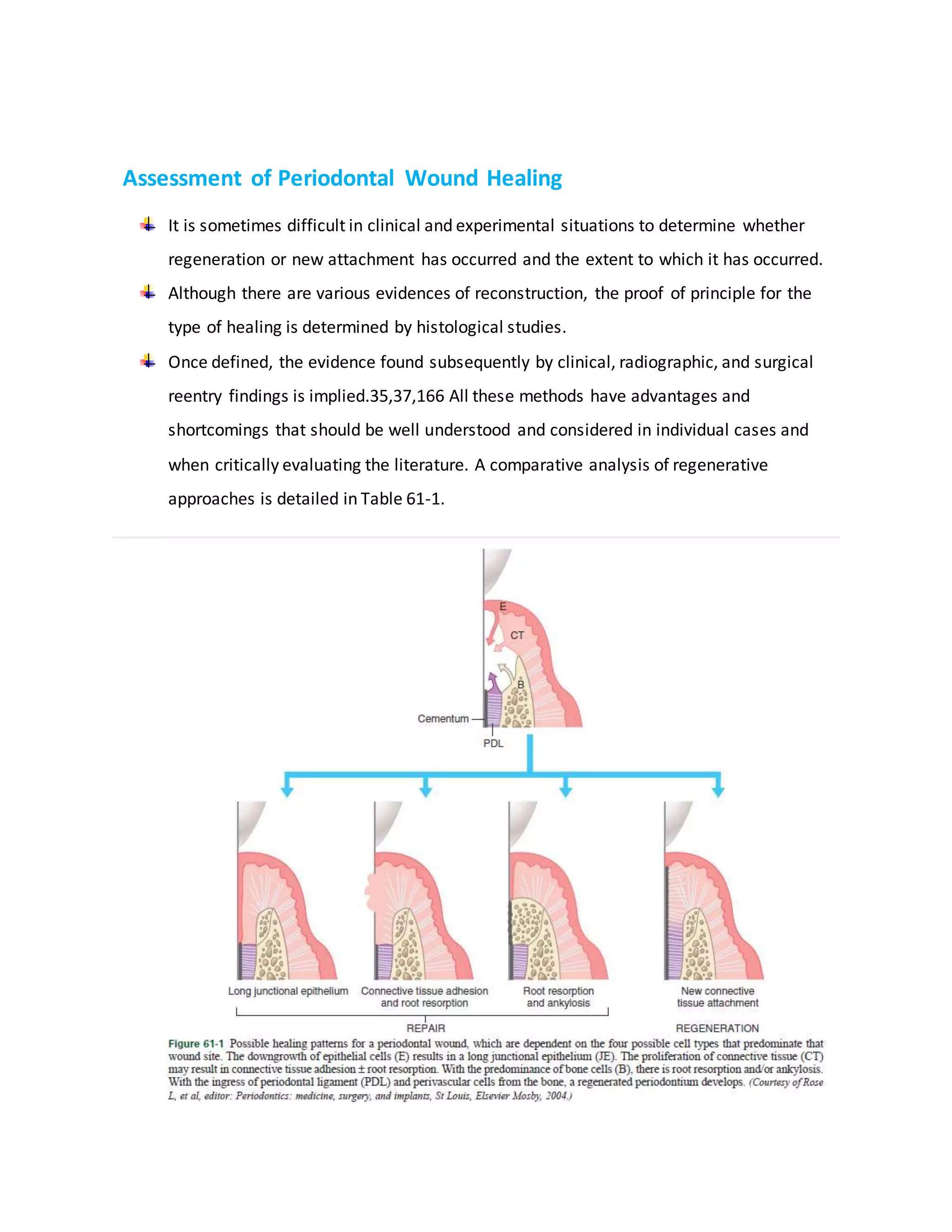
![“Bio-Oss:
“anorganic, osteoconductive, porous bone mineral matrix from bovine
cancellous or cortical bone.”
“Physical feature
trabecular architecture and porosity
permit clot stabilization and revascularization
allow for migration of osteoblasts, leading to osteogenesis.”
“Non Bone Graft Materials
Sclera, dura, cartilage, cementum, dentin, plaster of
paris, plastic materials, ceramics and coral derived
materials.
Not a reliable substitute.”
“Cartilage:
serves as a scaffolding, received limited evaluation”
“Plaster of Paris [calcium sulfate] :
biocompatible, porous, allowing fluid exchange, resorbs
completely in 1 to 2 weeks.
Usefulness in human studies not proved”
“Plastic material :
composite of Polymethyl-methacrylate and Polyhydroxyethylmethacrylate”.](https://image.slidesharecdn.com/perioassigmnt-190516132736/75/Advanced-periodontal-regenerations-22-2048.jpg)
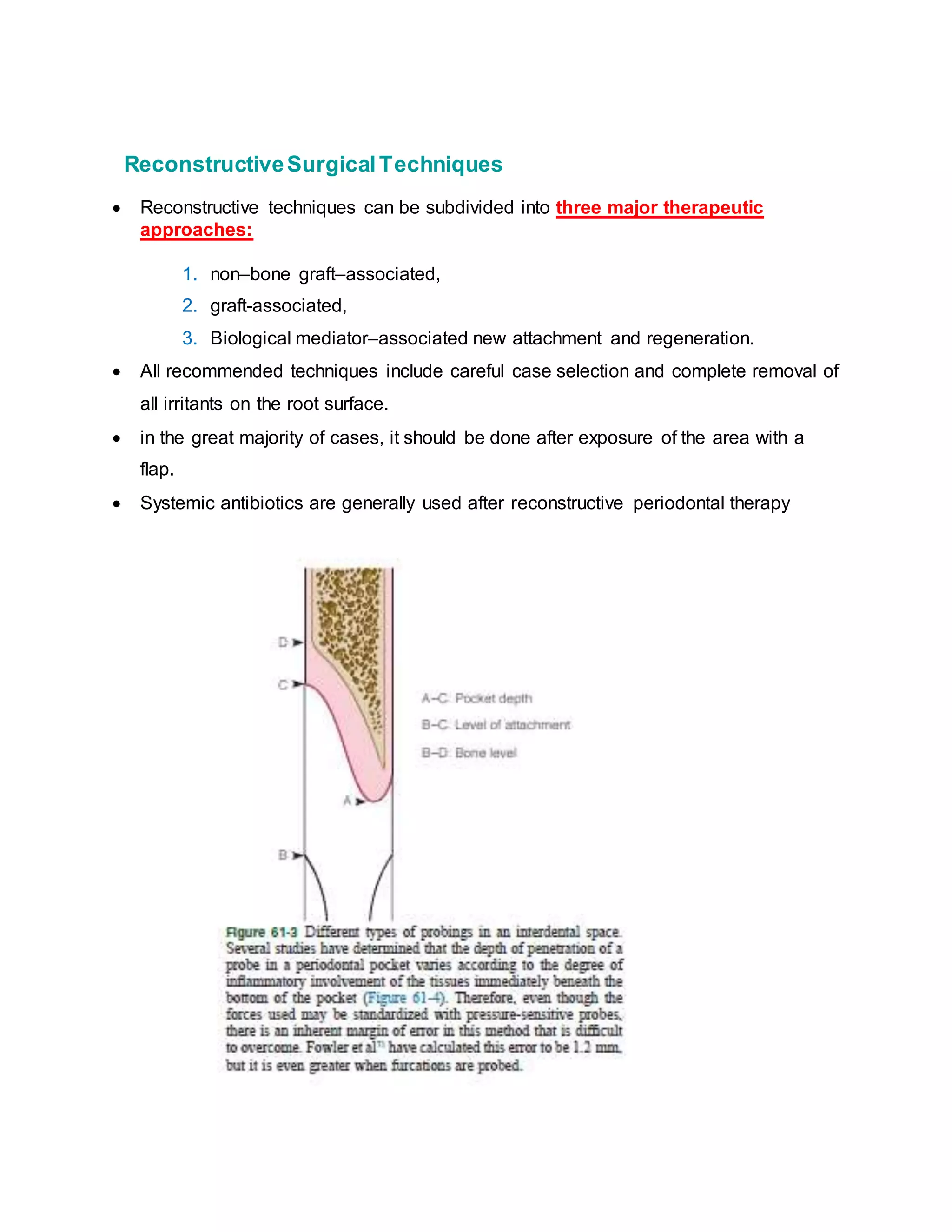
![“”Calcium Phosphate Biomaterial”
• “Osteoconductive, excellent tissue
biocompatibility, no inflammation or foreign body response.
• Two Types: Hydroxyapatite(HA): calcium : phosphate ratio :
1.67
• Tricalcium phosphate (TCP) : 1.5”
“Bioactive Glass
• Consist of: sodium and calcium salts, phosphates, and silicon
dioxide
• Used in the form of irregular particles measuring 90-170um or
300-355um
• When this material comes in contact with tissue fluids, the
surface of particles become coated with hydroxycarbonate apatite, incorporates organic
proteins such as chondroitin sulfate and glycosaminoglycans and attract osteoblast.”
“Coral Derived Material
Two types:
1. Natural coral [resorbed slowly-several months]
2. Coral derived porous hydroxyapatite [ years for
resorption]
Shows microscopic cementum and bone formation
But slow resorbability —limited clinical success””](https://image.slidesharecdn.com/perioassigmnt-190516132736/75/Advanced-periodontal-regenerations-23-2048.jpg)
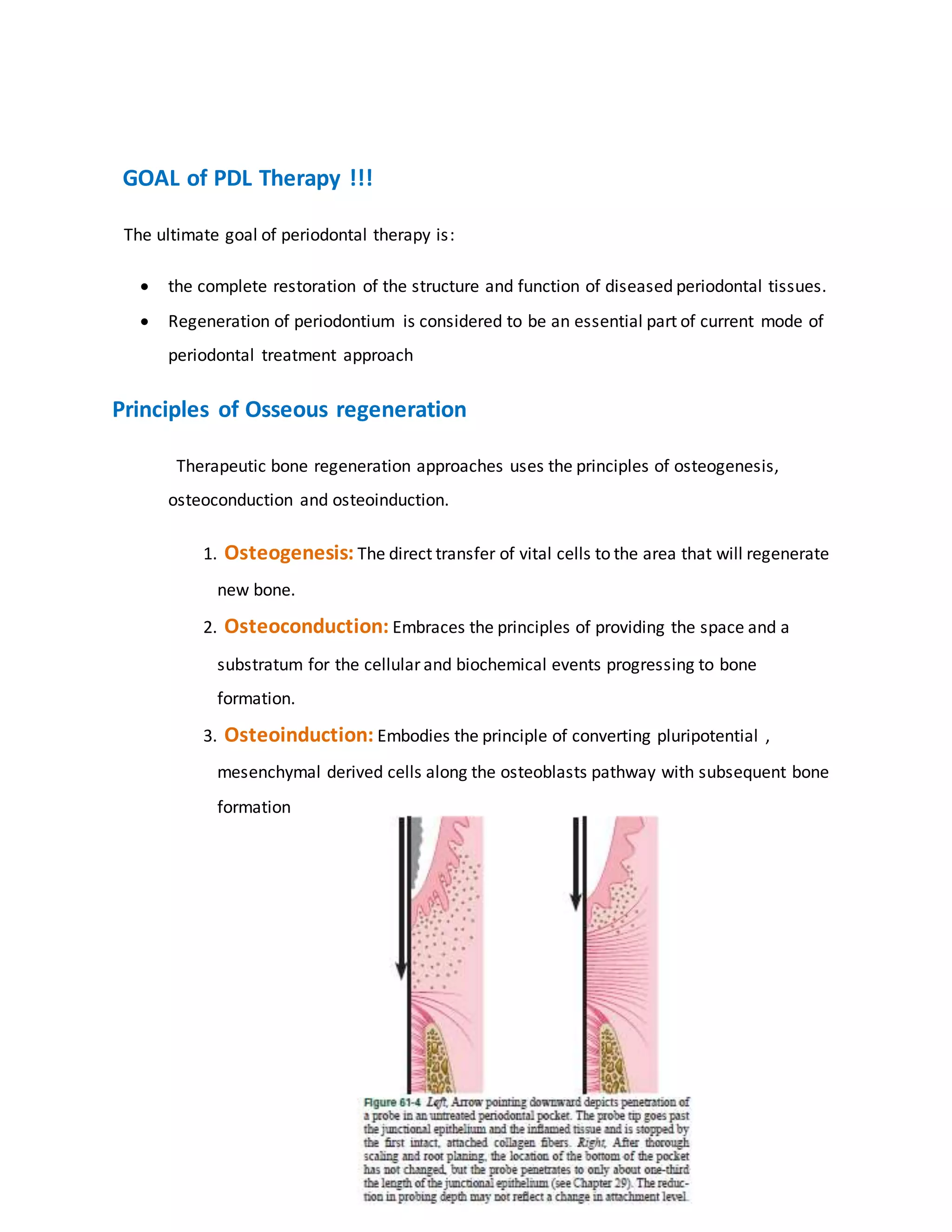
![“”Combined technique”
“Froum et al : criteria for choice of treatment”
“Clinical result depend upon:
• 1) dimension and morphology of defect( deeper>shallower)
• 2) number of walls
• 3) amount of root surface exposed and ability to obtain
adequate flap coverage
• 4) angle of defect with long axis of tooth (smaller – better)”
“Clinical Decision Tree
• For Deep, Well-Contained Defects—EMD alone, CAF (if necessary)
• For Moderate-Deep, Noncontained defects- EMD+Graft, CAF(if
necessary)
• For Supracrestal Defects with a shallow Vertical Defect-
EMD+Graft+Barrier membrane, with Coronally Advanced Flap”
“EMD- enamel matrix derivative. Emdogain [Froum et al 2001] »](https://image.slidesharecdn.com/perioassigmnt-190516132736/75/Advanced-periodontal-regenerations-24-2048.jpg)
