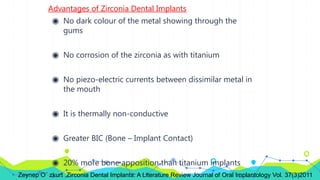
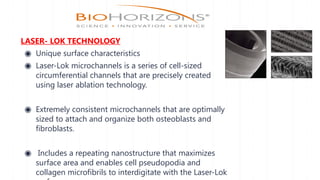
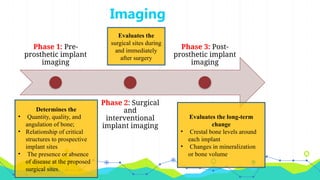
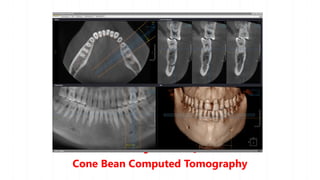
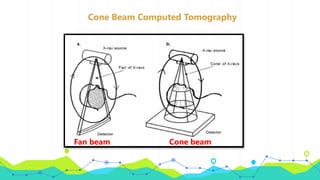
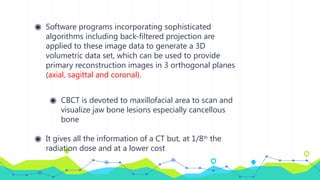
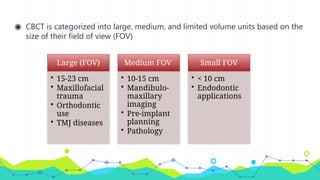
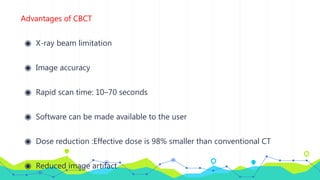
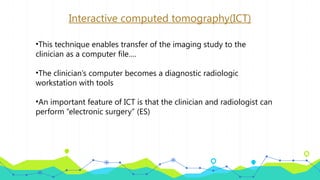
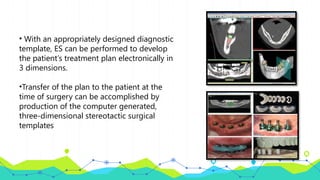
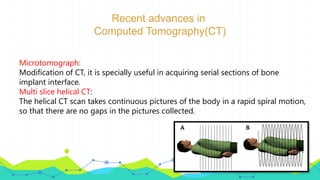
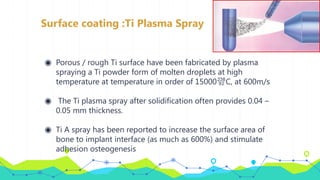
The document discusses recent advancements in implantology, covering topics such as diagnostic imaging, implant design, materials, and rehabilitation concepts. It highlights improvements in imaging techniques like CBCT and TAC, new implant designs including mini and short implants, and material innovations enhancing osseointegration. The findings demonstrate the effectiveness and high survival rates associated with modern implants and techniques in dental practice.







![Hydroxyapatite coatings
◉ Hydroxyapatite [Ca10(PO4)6OH]2 coating was brought to the
dental profession by DeGroot
◉ HA forms a strong chemical bond with bone due to the
presence of free calcium and phosphate compounds at the
implant surface
◉ The HA coating consists of amorphous and crystalline forms
with a large density of cracks.
◉ The top 1-2 µm of the HA layer being amorphous, while the
rest of the crystalline layer is hexagonally packed](https://image.slidesharecdn.com/recentadvancesinimplants-240824082457-da6784d1/85/recent-advances-in-implants-in-dentistry-pptx-54-320.jpg)