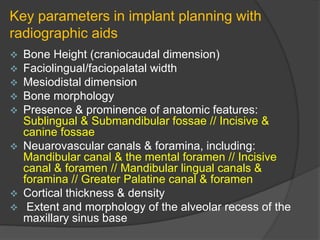
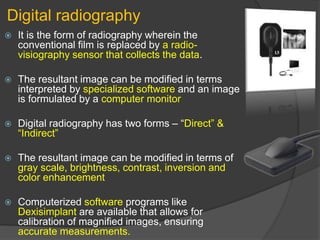
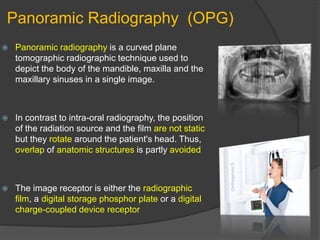
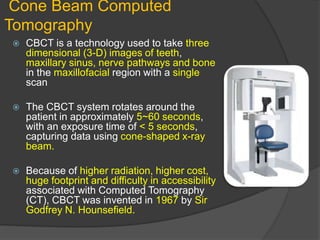
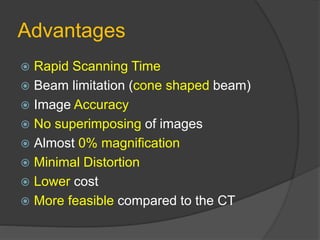
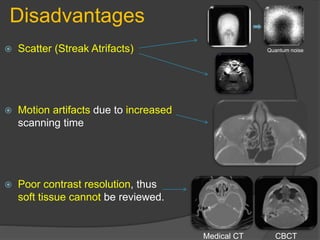
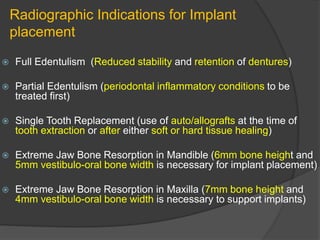
The document reviews the imaging modalities and techniques essential for dental implant procedures, discussing pre-surgical, surgical, and post-prosthetic imaging phases. It highlights the importance of various imaging types, such as digital radiography, panoramic radiography, and cone beam computed tomography, along with their indications, advantages, and disadvantages. Additionally, diagnostic imaging's role in assessing bone quality, anatomy, and patient-specific considerations for implant placement is emphasized.
![Introduction
The term “implant” itself remains ambiguous.
According to the Academy of Osseointegration a
dental implant is defined as “an artificial material or
tissue that shows biocompatibility upon its surgical
implantation.” [this definition has been authorized
by American College of Prosthodontists & American
Academy Of Periodontology]
According to GPT 8 – Any object or material such
as an alloplastic or other tissue, which is partially or
completely inserted or grafted into the body for
therapeutic, diagnostic, prosthetic or experimental
purposes.](https://image.slidesharecdn.com/radiographicconsiderationsindentalimplants-200522185923/85/Radiographic-considerations-in-dental-implants-3-320.jpg)