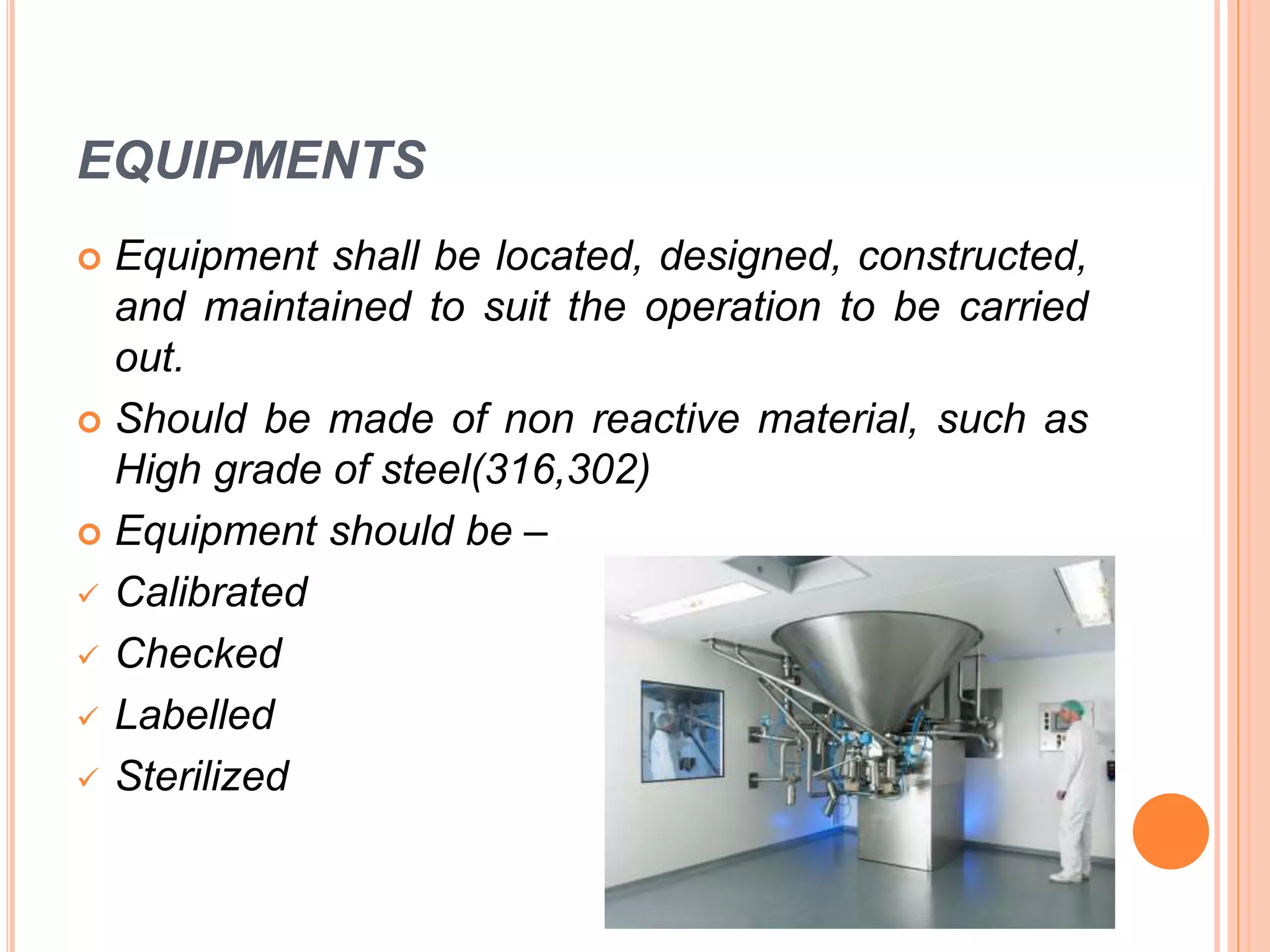
The document discusses the history and principles of Good Manufacturing Practices (GMP). It originated after mass poisonings from contaminated drugs in the early 1900s. GMP aims to ensure consistent production of safe medicines through guidelines covering facilities, equipment, personnel, documentation, raw materials, production, and quality control. Major regulations include those from the US FDA, EU, and India. Following GMP principles during pharmaceutical manufacturing helps protect patient health.