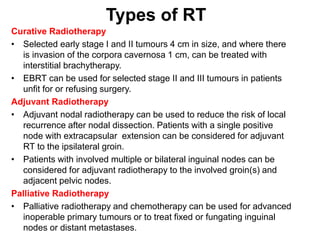
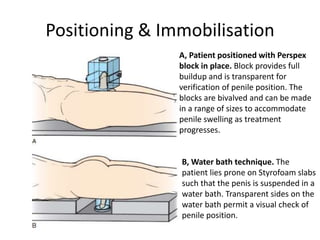
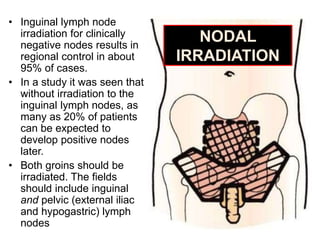
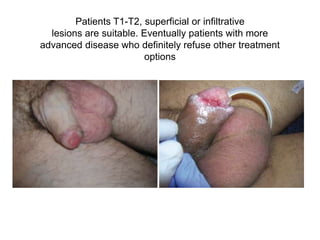
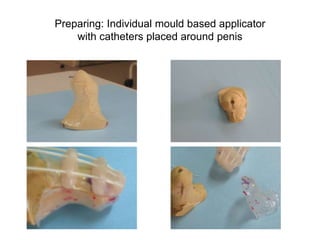
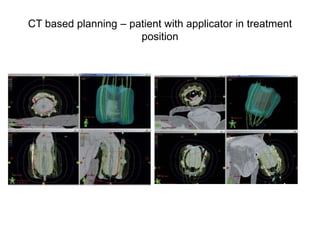
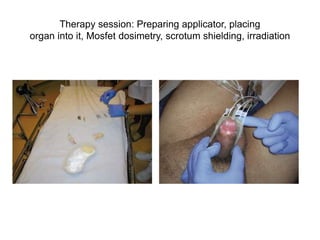
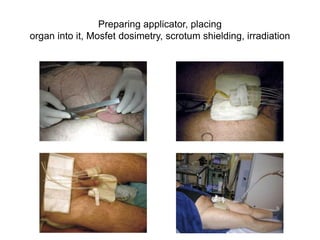
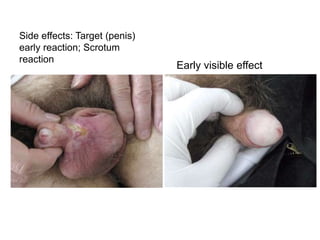
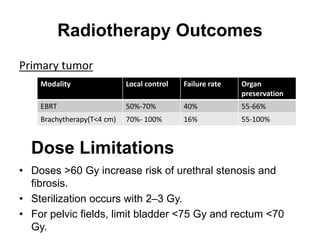
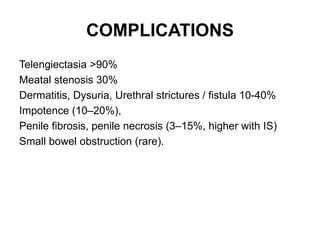
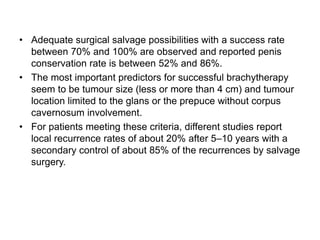
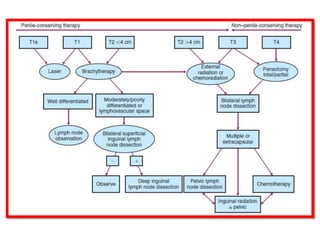
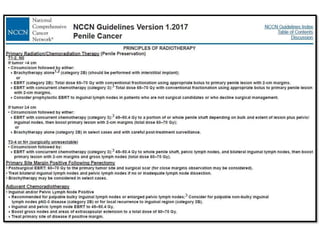
Radiotherapy is an important treatment option for penile carcinoma. It can be used as curative treatment for early stage tumors, as adjuvant treatment after surgery to reduce the risk of recurrence, and for palliation of advanced tumors. The main radiotherapy techniques are external beam radiotherapy and brachytherapy. Brachytherapy involves placing radioactive sources inside or next to the tumor and is often used for small early stage tumors, providing good tumor control rates and organ preservation. External beam radiotherapy uses external radiation beams and can treat larger tumors or be used as adjuvant therapy. Proper patient positioning and immobilization is important for both techniques to precisely target the tumor while sparing surrounding organs. Radiotherapy is generally well-tol