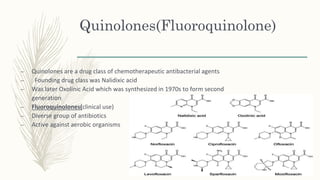
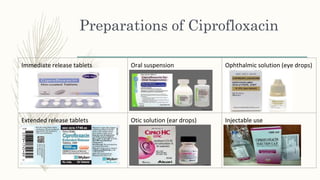
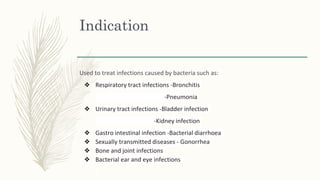
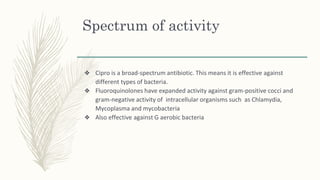
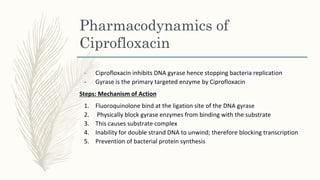
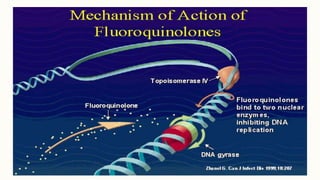
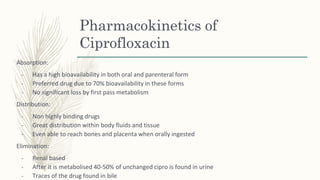
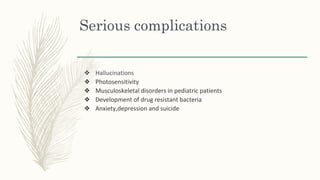
Quinolones are a class of antibiotics that includes ciprofloxacin. Ciprofloxacin is effective against both gram-positive and gram-negative bacteria. It works by inhibiting the DNA gyrase enzyme and preventing bacterial replication. While generally safe and effective, overuse has led to increasing antibiotic resistance. Alternative treatments include trimethoprim, levofloxacin, and ampicillin. Proper use and public health measures are needed to prevent further development of resistance.