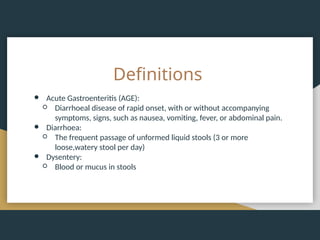
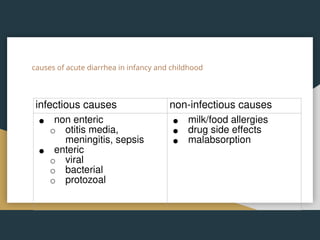
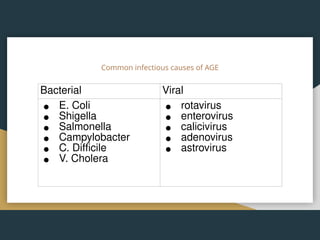
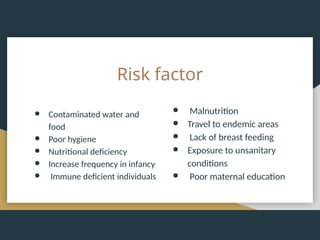
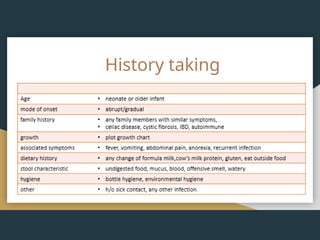
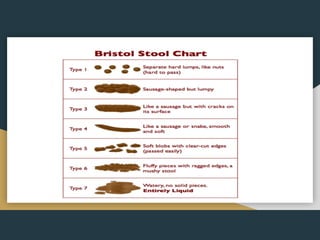
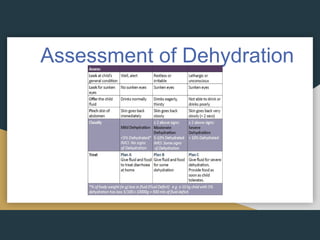
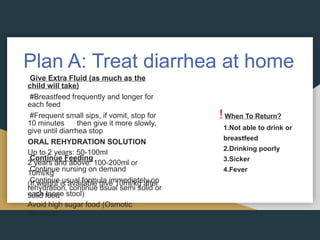
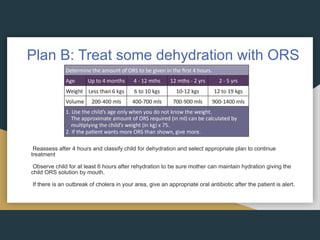
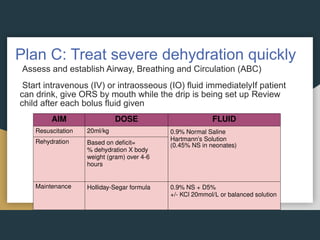
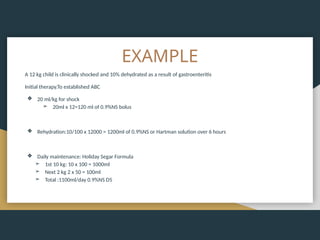
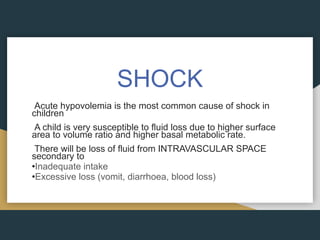
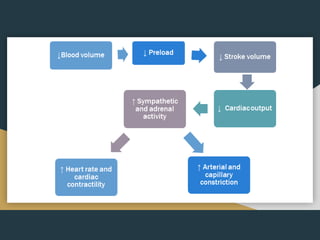
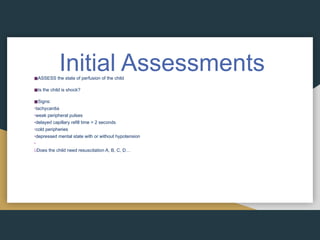
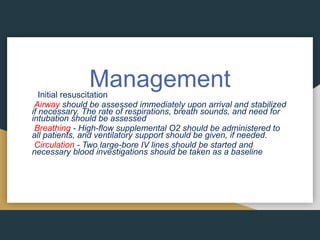
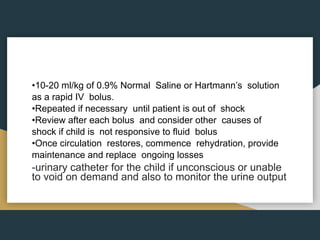
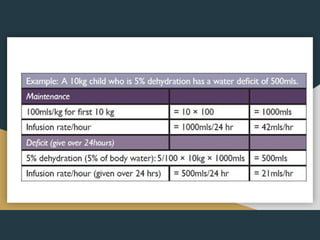
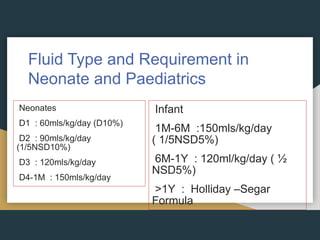
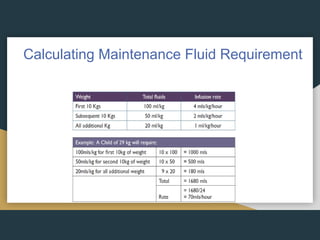
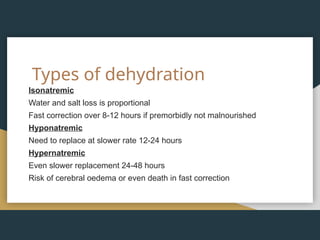
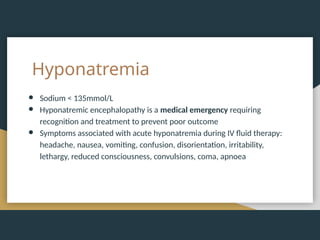
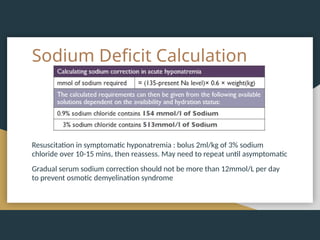
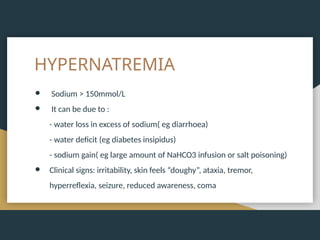
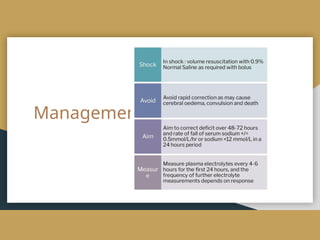
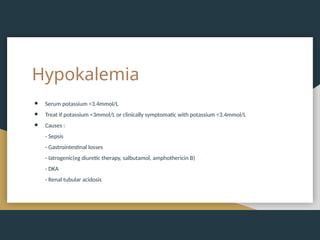
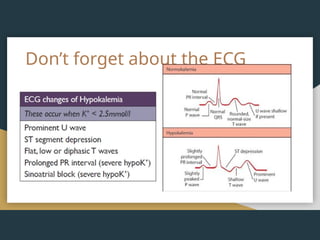
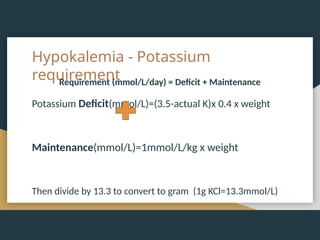
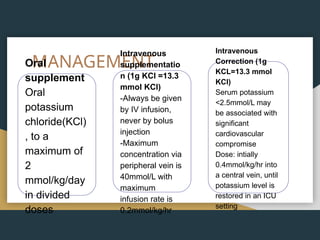
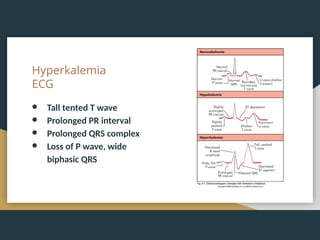
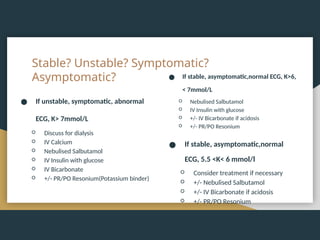
The document discusses acute gastroenteritis, detailing definitions, causes, symptoms, and management strategies, particularly fluid and electrolyte management. It outlines treatment plans for various levels of dehydration, including home treatment, oral rehydration solutions, and intravenous therapies for severe cases. Additionally, the document highlights the importance of monitoring electrolyte imbalances and provides management guidelines for conditions like hyponatremia and hyperkalemia.