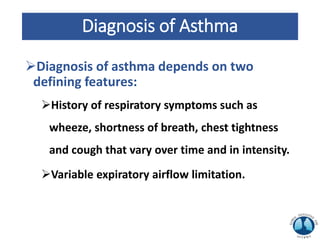
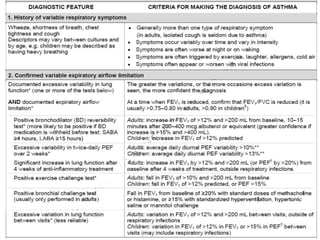
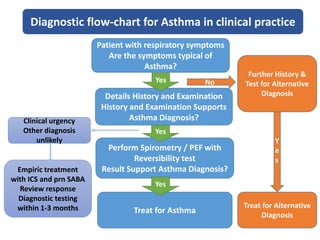
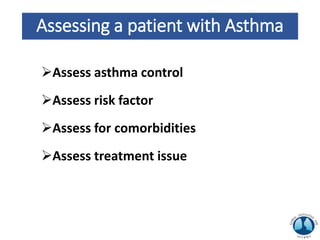
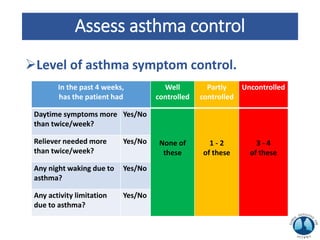
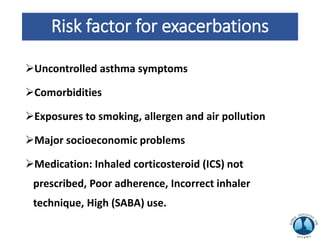
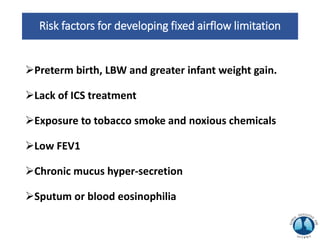
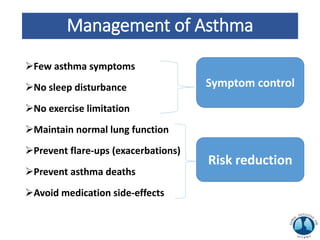
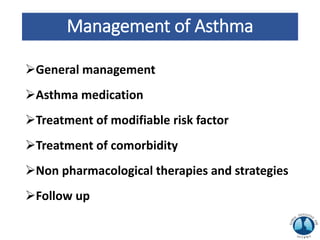
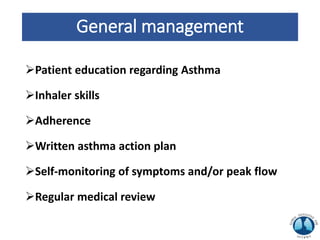
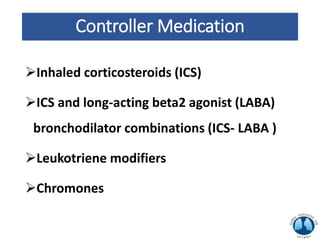
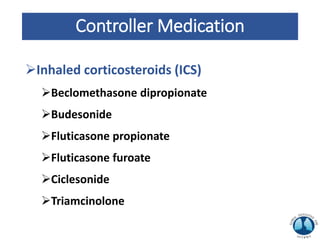
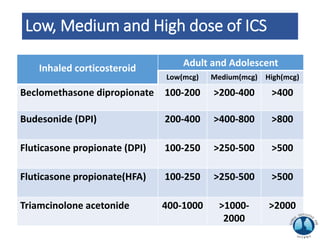
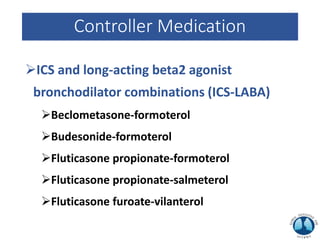
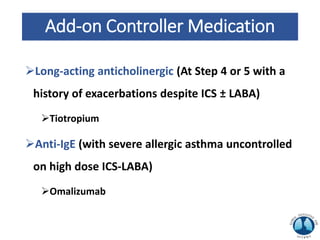
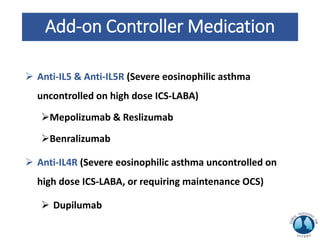
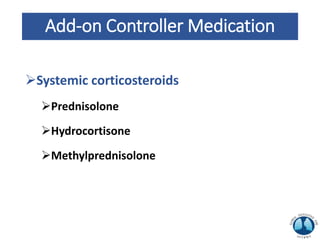
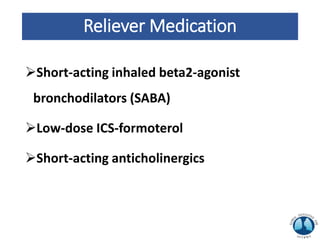
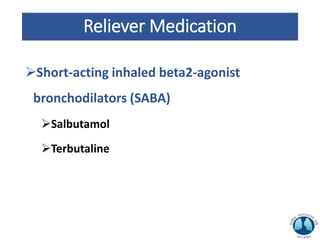
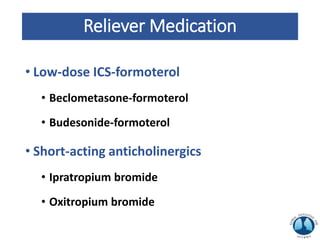
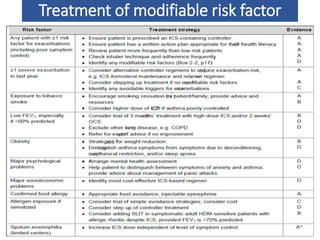
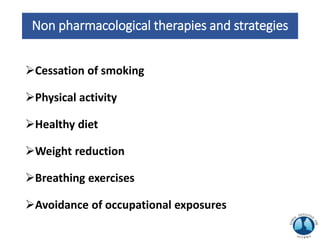
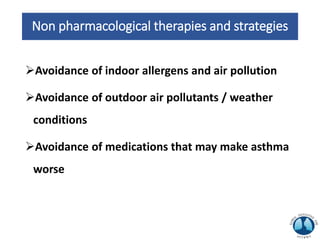
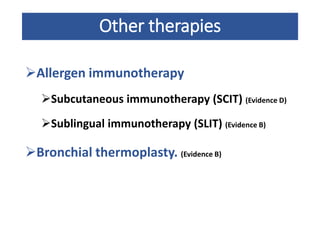
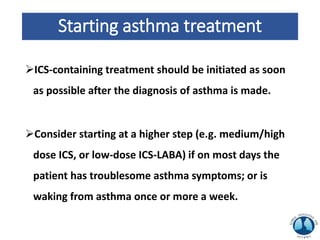
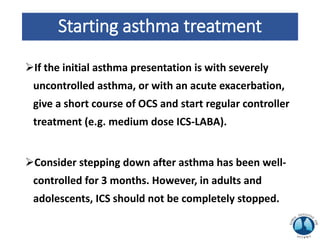
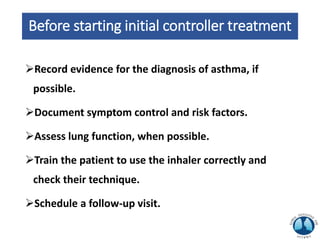
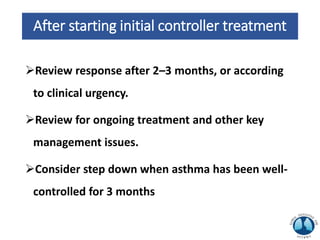
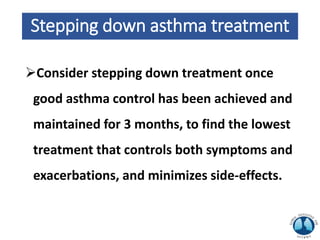
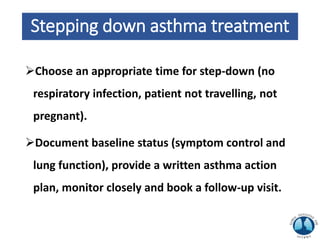
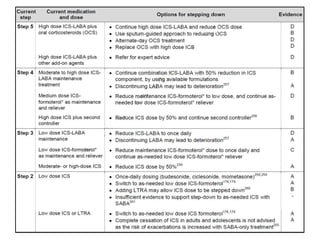
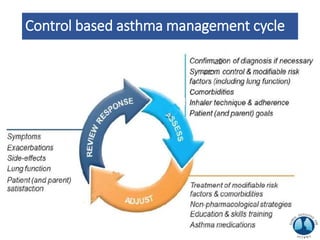
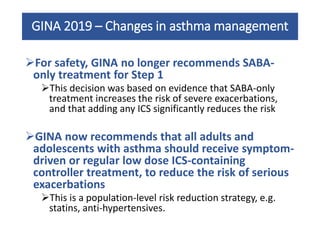
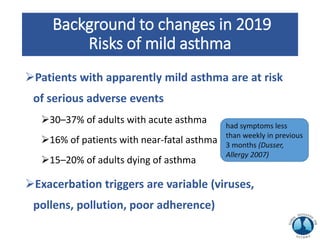
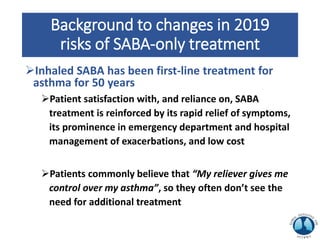
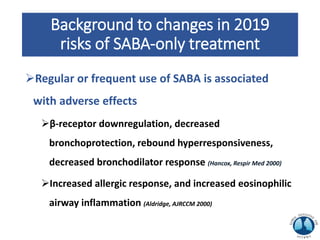
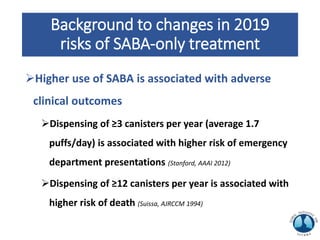
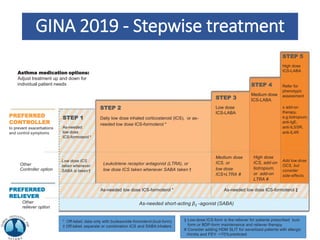
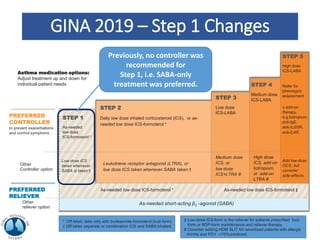
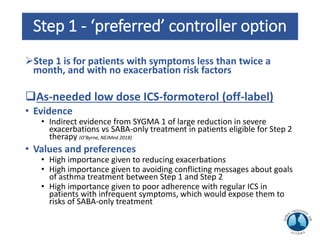
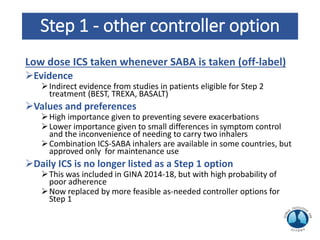
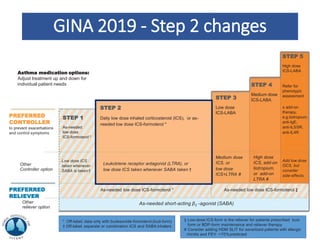
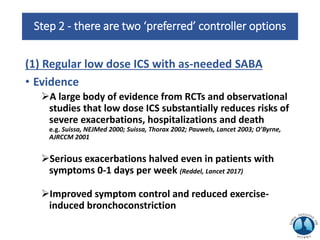
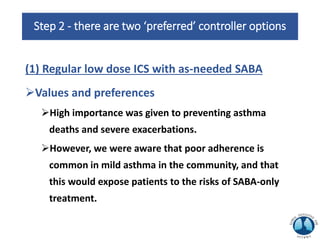
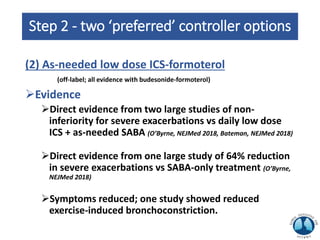
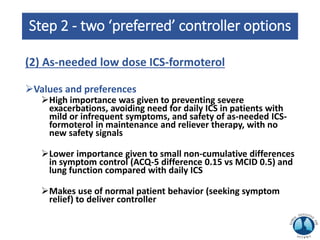
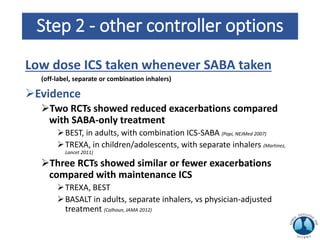
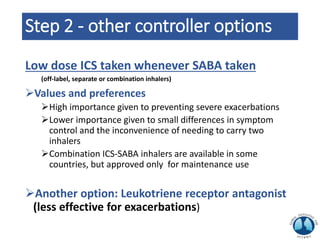
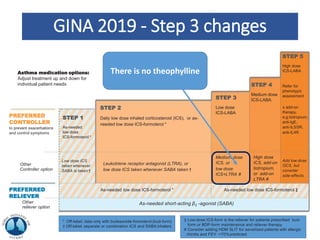
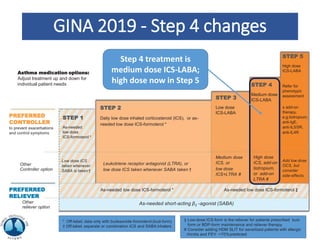
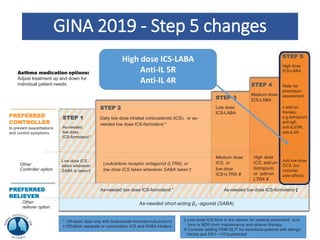
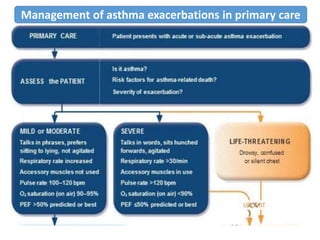
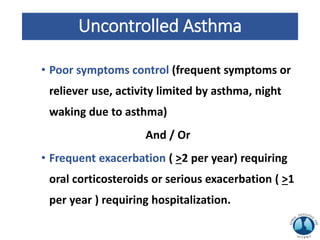
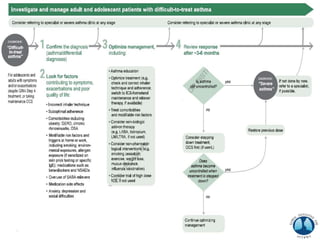
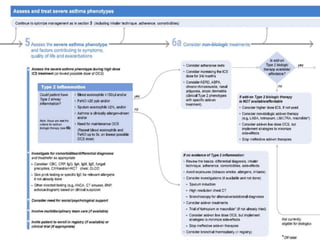
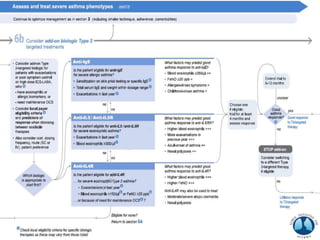
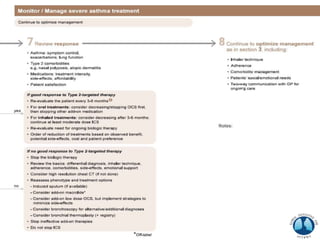
The document provides an overview of the Global Initiative for Asthma's 2019 strategy for asthma management and prevention. It discusses GINA's goals of reducing asthma prevalence, morbidity, and mortality. It also summarizes the key aspects of asthma including phenotypes, diagnosis, assessment of control and risk factors, and pharmacological and non-pharmacological treatment strategies. The treatment approach involves classifying asthma severity and control to determine the appropriate controller medications and adjusting the treatment regimen up or down as needed.