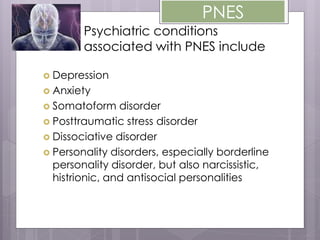
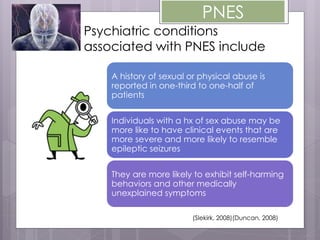
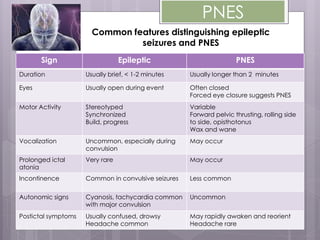
Psychogenic nonepileptic seizures (PNES) are not caused by neurological dysfunction but are psychologically determined. Common psychiatric conditions associated with PNES include depression, anxiety, somatoform disorder, PTSD, dissociative disorder, and various personality disorders. A history of sexual or physical abuse is reported in one-third to half of PNES patients. PNES episodes typically last longer than 2 minutes, involve eyes being closed and variable motor movements rather than stereotyped behaviors seen in epilepsy. Diagnosis involves distinguishing PNES from epileptic seizures based on clinical features during and after episodes.