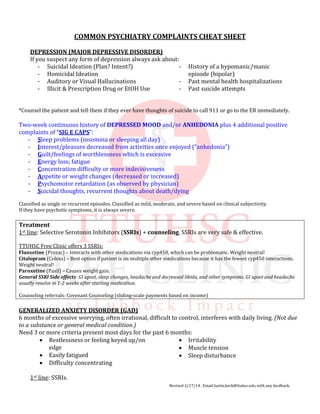
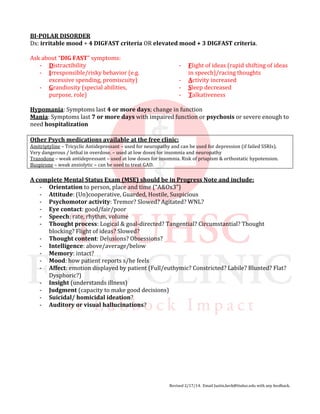
The document is a psychiatry cheat sheet outlining key points for assessing and treating major depressive disorder, generalized anxiety disorder, and bipolar disorder. It emphasizes the importance of evaluating suicidal ideation and other symptoms, and recommends SSRIs as first-line treatment. It also includes a guide for conducting a complete mental status exam.