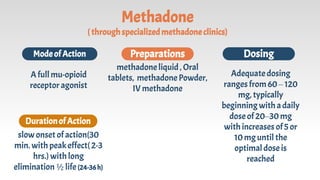
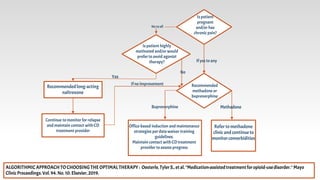
The document discusses addiction replacement therapy (also known as opioid substitution therapy) for treating opioid use disorder. It begins by outlining the objectives and magnitude of the global and Egyptian opioid problems. It then describes medication-assisted treatment using opioid agonists/antagonists like methadone and buprenorphine. The benefits of opioid substitution therapy include reducing illegal opioid use and associated harms while increasing social functioning. Common myths about substitution therapy are addressed. Treatment algorithms are provided to guide patient assessment and selection of optimal replacement therapies like methadone, buprenorphine or naltrexone based on their different pharmacological profiles and patient characteristics.