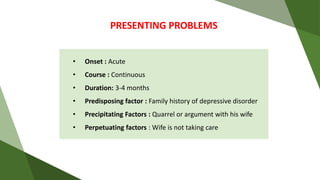
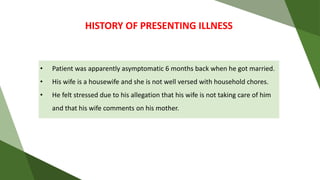
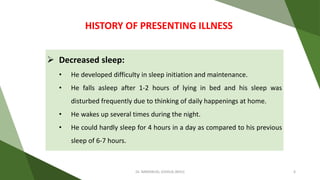
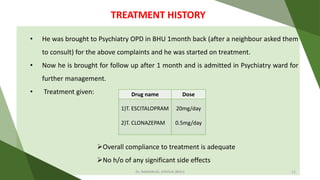
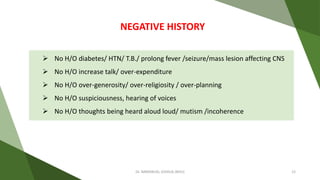
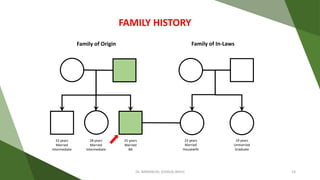
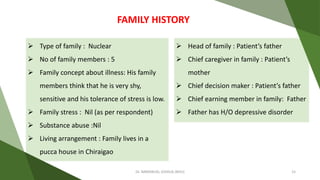
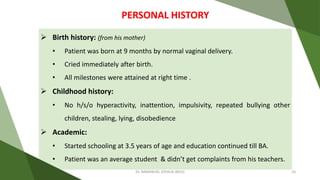
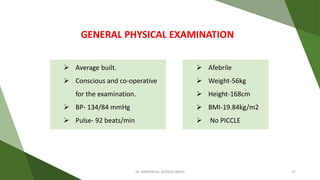
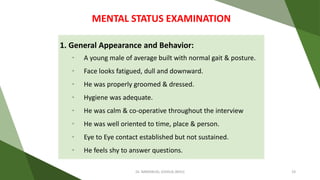
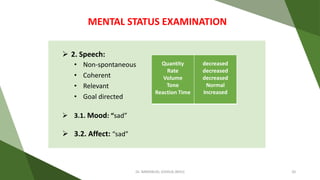
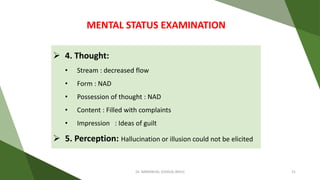
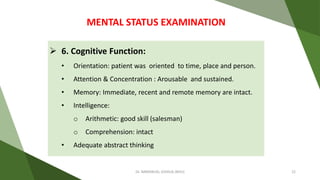
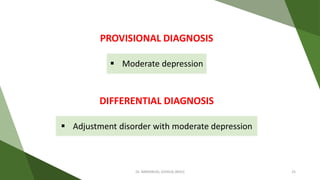
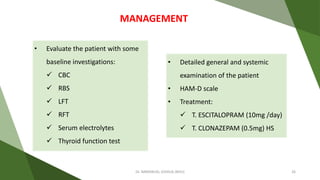
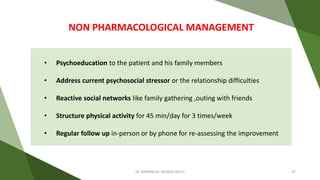
A 25-year-old male presents with symptoms of moderate depression, including decreased sleep, appetite, sadness, loss of interest, and guilt ideas, which have persisted for 3-4 months following marital stressors. His family history includes a father with a depressive disorder, and he was treated with escitalopram and clonazepam, showing adequate compliance. Non-pharmacological management recommendations include psychoeducation, addressing psychosocial stressors, and structured physical activity.