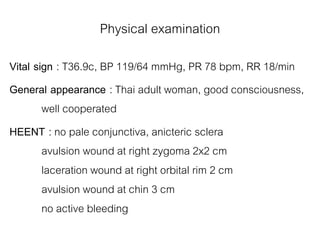
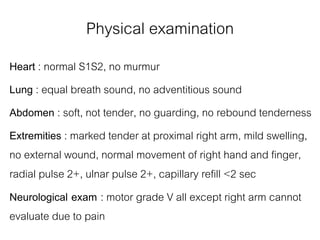
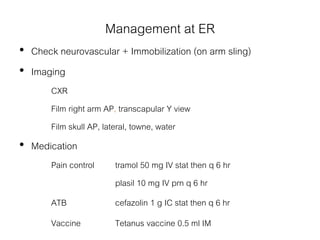
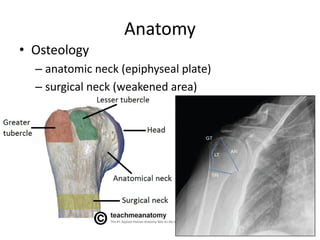
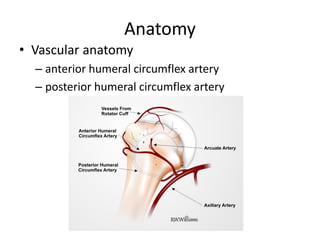
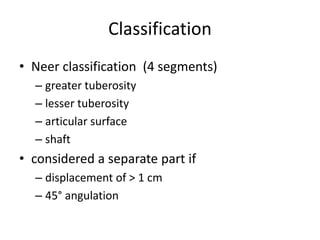
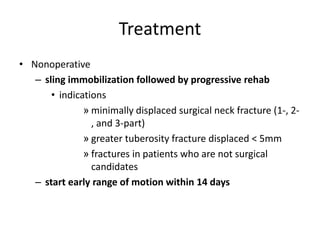
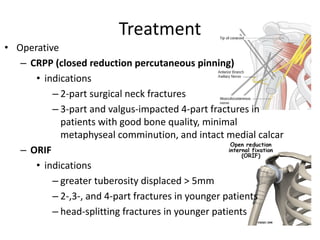
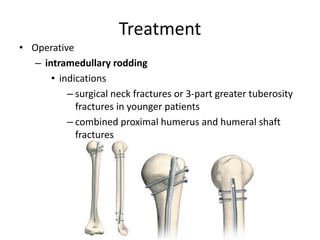
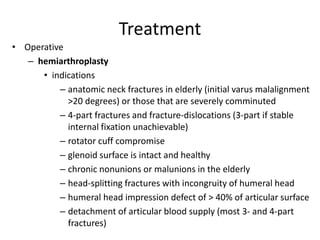
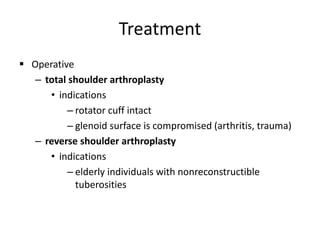
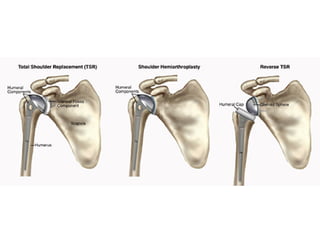
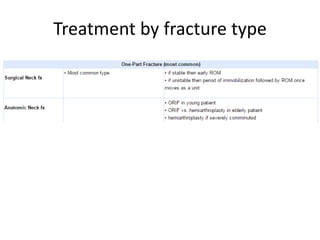
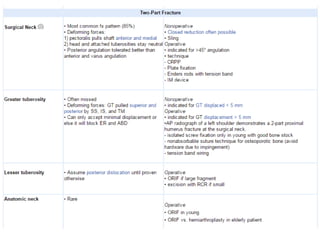
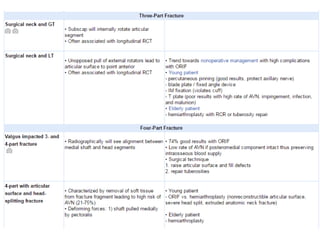
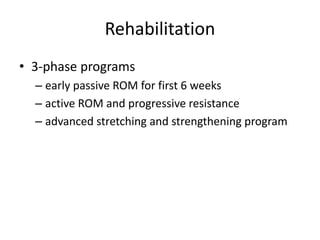
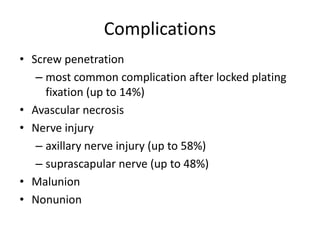
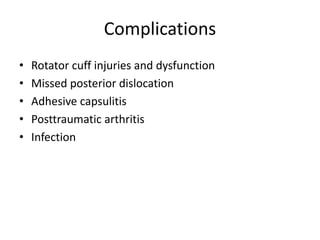
This document summarizes the key points about a proximal humerus fracture case. It describes a 30-year-old female patient who was brought to the emergency room after falling off her motorcycle. Her injuries included a proximal humerus fracture on her right arm. The document reviews the epidemiology, anatomy, classification, evaluation, treatment options and rehabilitation for proximal humerus fractures. It provides details on the patient's case, management in the emergency room, and anticipated treatment plan.