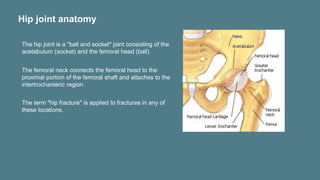
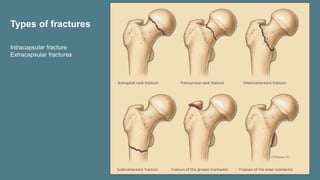
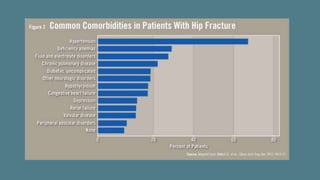
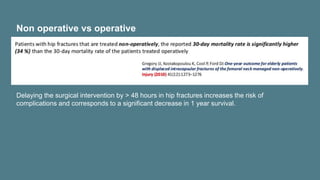
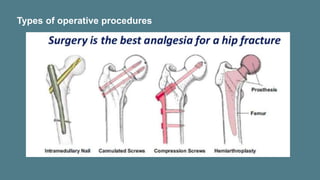
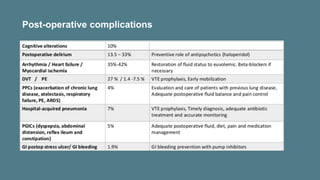
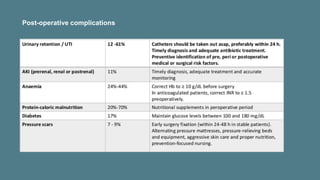
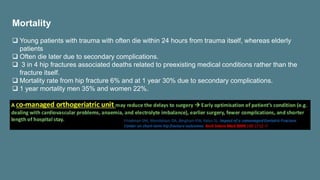
This document discusses hip fractures in geriatric patients. It begins by introducing that hip fractures are increasing as the population ages and outlines risk factors like osteoporosis and falls. It then describes hip anatomy and the different types of fractures. Risk factors for falls and fractures are explained. The importance of timely surgery within 48 hours is highlighted. Post-operative complications and the high mortality rate associated with hip fractures in elderly patients are also summarized.