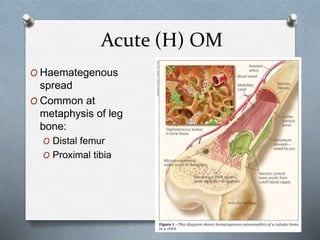
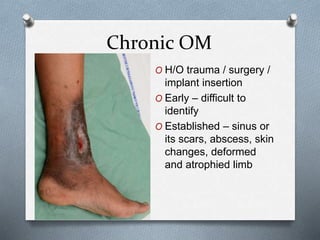
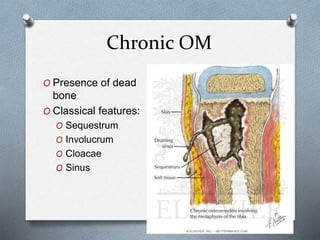
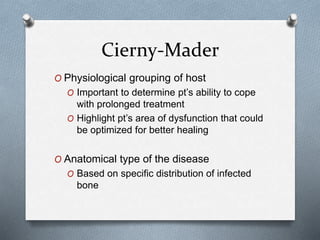
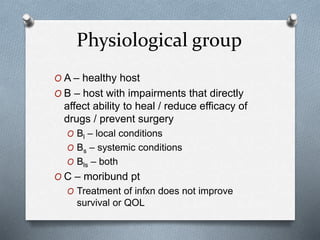
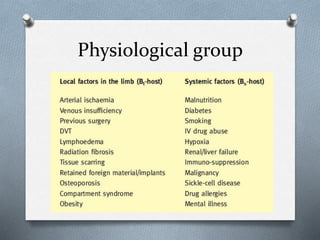
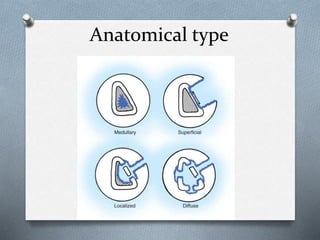
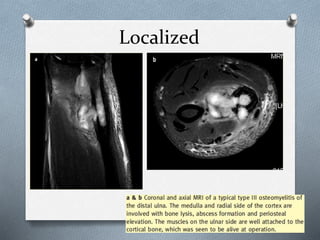
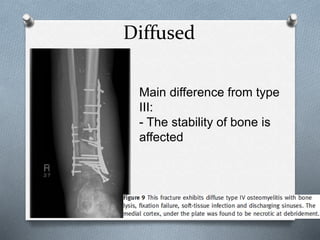
This document discusses the classification and approach to osteomyelitis (OM). It notes that OM is becoming more common due to secondary causes like surgery, injury, and diabetes. The document outlines the differences between acute and chronic OM, signs and symptoms to look for, common locations, and characteristics of each type. It recommends investigations and cultures if OM is suspected. The key classification discussed is the Cierny-Mader system, which considers the physiological health of the patient and the anatomical location and spread of the infected bone to determine the appropriate treatment approach.