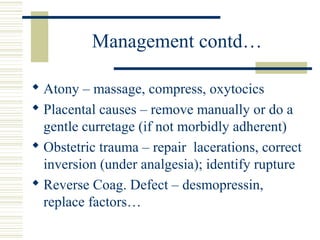
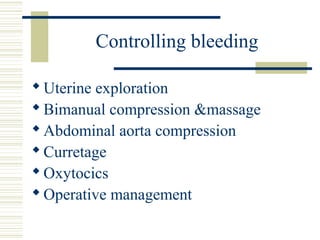
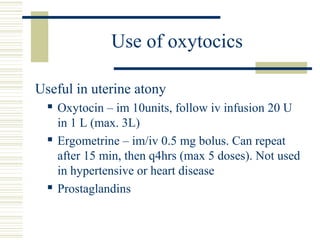
Postpartum hemorrhage (PPH) is defined as blood loss exceeding 500 ml after vaginal delivery within 24 hours. It is a leading cause of maternal mortality, especially in resource-poor settings. Risk factors include polyhydramnios, macrosomia, prolonged labor, and previous surgery. Management involves resuscitation, assessing uterine contraction, exploring the uterus, and administering oxytocics for atony or performing manual removal of placental tissue. Prevention strategies include active management of the third stage of labor with oxytocics immediately after delivery and risk assessment during antenatal care.