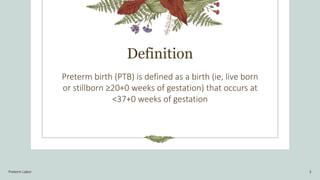
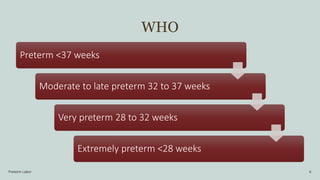
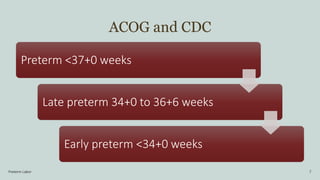
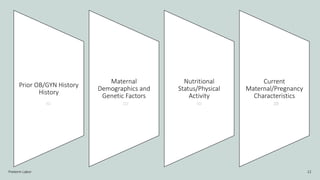
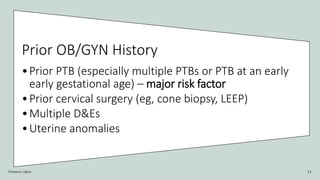
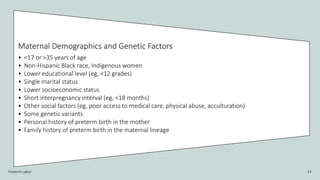
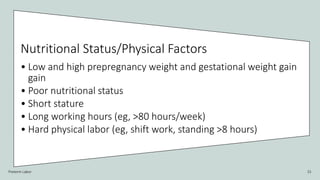
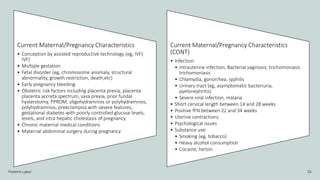
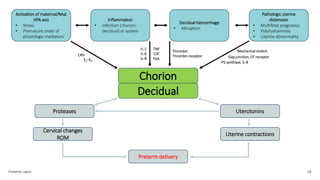
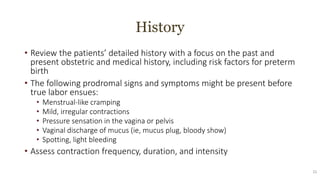
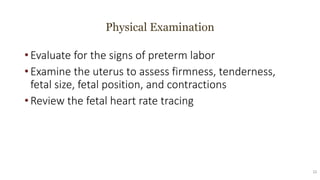
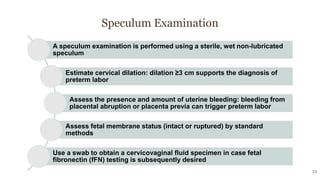
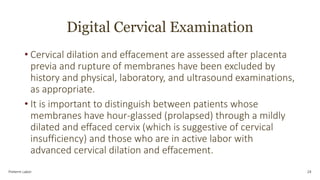
The document discusses preterm birth (PTB), defined as a birth occurring before 37 weeks of gestation, and its classification, risk factors, and management. It highlights the significance of identifying preterm labor through diagnostic evaluations such as history, physical examination, and ultrasonography, along with criteria for diagnosis. Management strategies include administering antenatal corticosteroids, tocolytics, and antibiotics, alongside interventions for specific patient presentations.