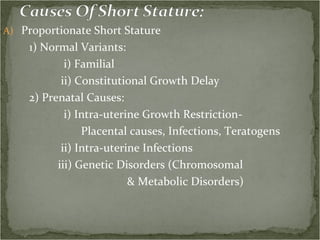
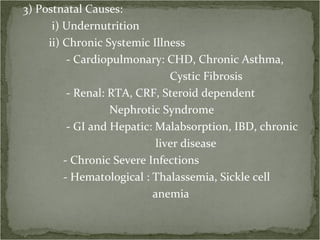
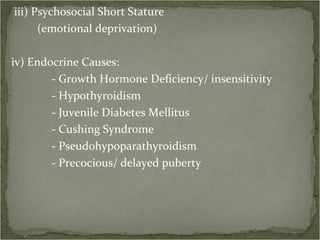
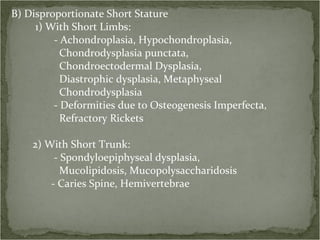
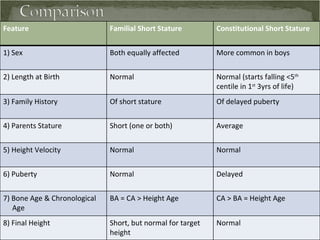
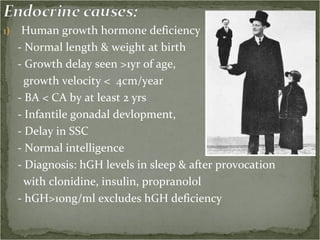
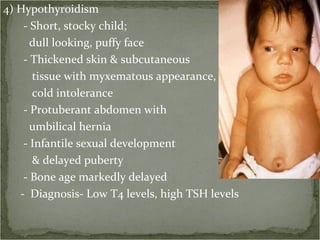
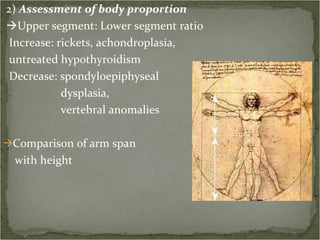
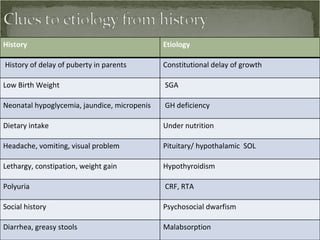
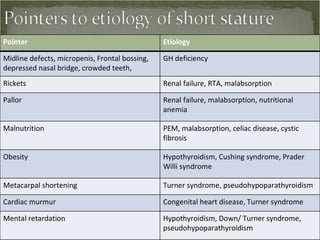
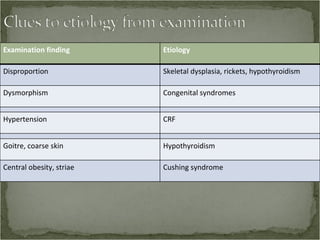
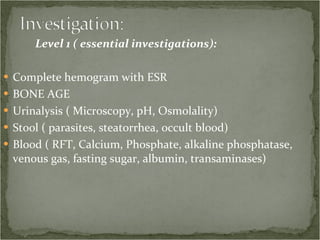
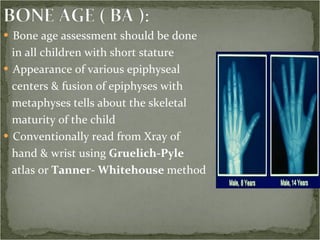
Approximately 3% of children are short, with half being physiologically short due to familial or constitutional factors, and half being pathologically short. Common causes of pathological short stature include genetic disorders, chronic illnesses, malnutrition, and endocrine disorders such as growth hormone deficiency or hypothyroidism. A thorough evaluation includes medical history, physical examination, assessment of growth parameters, bone age, and laboratory tests to identify the underlying cause.