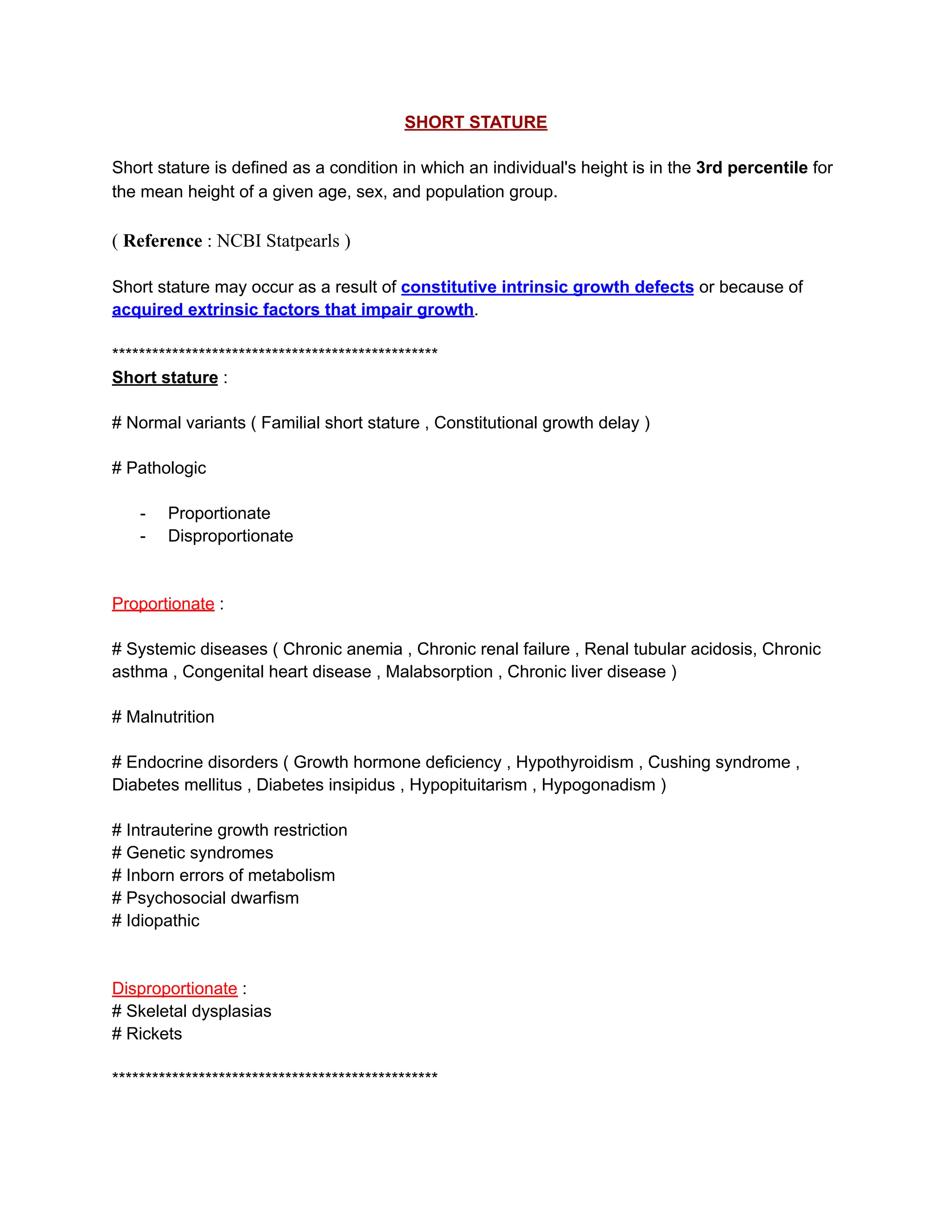
Short stature is defined as a height below the 3rd percentile for a specific age and population, resulting from intrinsic growth defects or extrinsic factors. It can be categorized into normal variants and pathological causes, with various underlying systemic, nutritional, or genetic conditions leading to growth impairment. Diagnosis involves evaluating growth patterns, skeletal maturation, and potentially conducting laboratory tests to assess growth hormone function, with treatment options including recombinant growth hormone therapy for those with deficiencies.