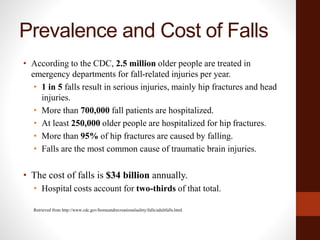
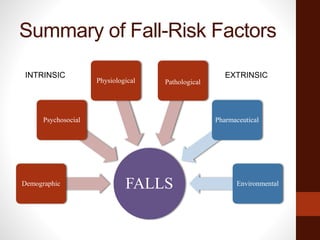
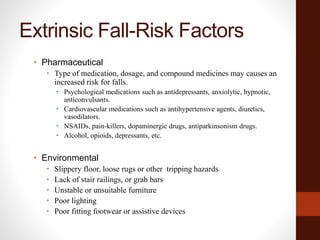
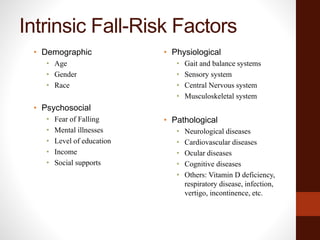
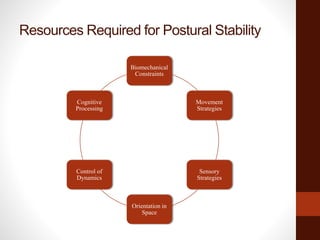
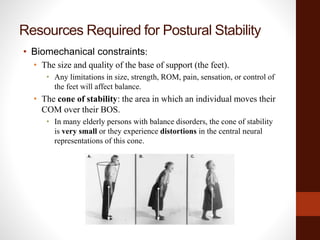
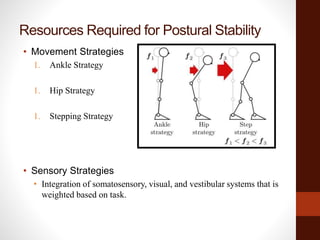
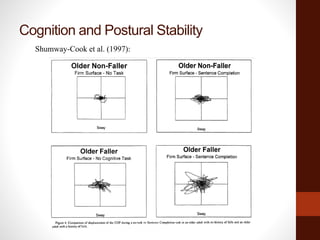
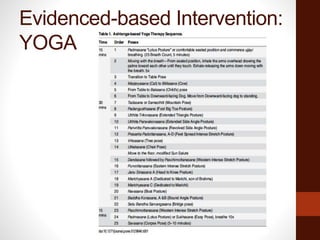
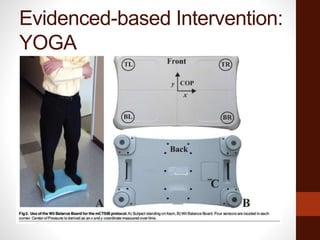
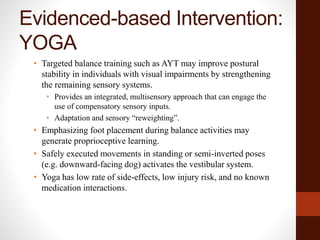
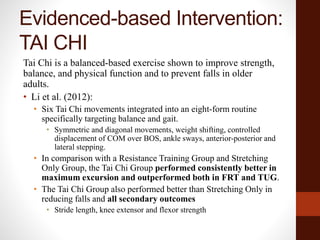
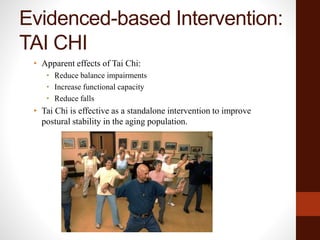
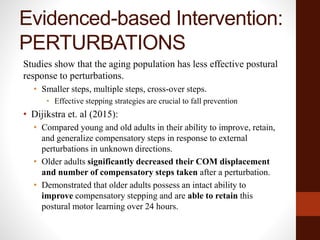
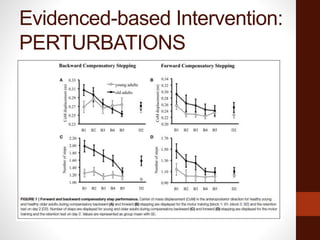
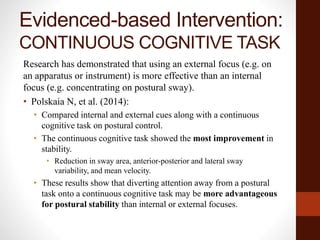
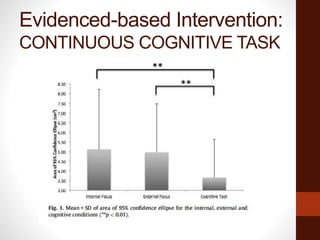
The document provides an overview of postural instability and falls in the aging population. It defines key terms, discusses prevalence and risk factors for falls, and describes the relationship between postural instability and falls. Maintaining postural stability requires the integration of multiple sensory, motor, and cognitive systems. Evidence-based interventions that have been shown to improve postural stability and reduce falls in older adults include yoga, Tai Chi, and exercises challenging balance.