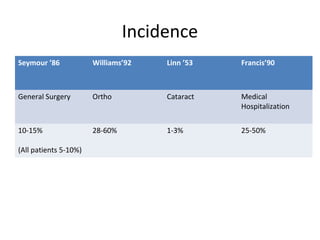
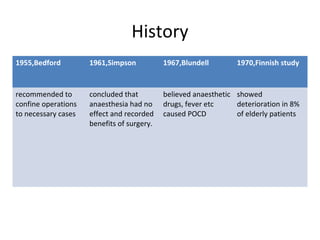
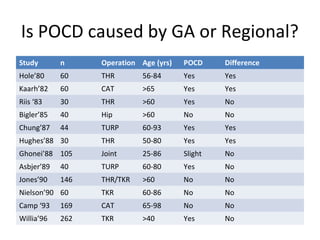
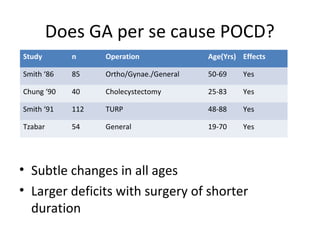
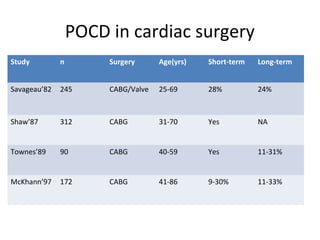
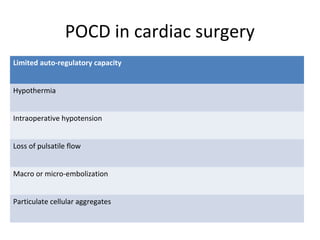
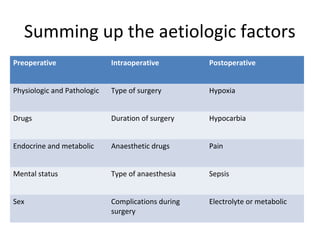
Postoperative Cognitive Dysfunction (POCD) in elderly patients is characterized by changes in personality, social integration, and cognitive abilities following surgery. Studies have found POCD incidence rates ranging from 10-60% in elderly patients after various surgeries like general surgery, orthopedic surgery, and cataract surgery. POCD is thought to be caused by physiological effects of anesthesia like hyperventilation and hypotension, as well as genetic factors and surgery-related stress. Both general anesthesia and regional anesthesia may contribute to POCD, though results from studies comparing the two have been mixed. Preoperative, intraoperative, and postoperative factors like the type and duration of surgery, anesthesia drugs used, pain, and hypoxia may