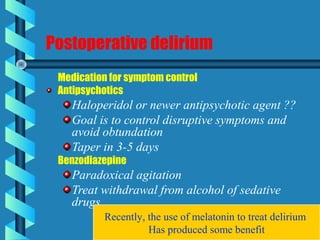
Elderly patients are at increased risk of postoperative complications such as delirium, cognitive dysfunction, and hypotension. Preventive measures include preoperative assessment of organ function, maintaining normothermia intraoperatively, vigilant postoperative monitoring and pain control, and minimizing delirium risk factors such as cognitive impairment, medications, and medical issues. Regional anesthesia may provide benefits over general anesthesia by avoiding stress responses but does not necessarily reduce risks of cognitive issues.