The document discusses population health management (PHM) and its role in supporting integrated care systems (ICS) in the UK. Key points:
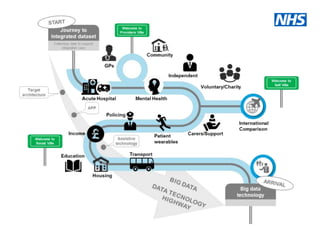
- ICSs will be established everywhere by 2021 to integrate primary/specialist care, physical/mental health, and health/social care.
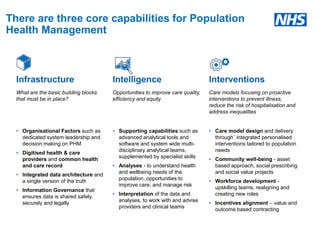
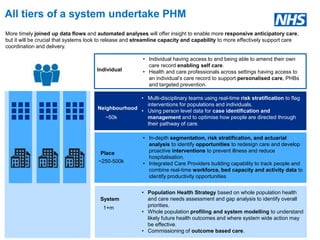
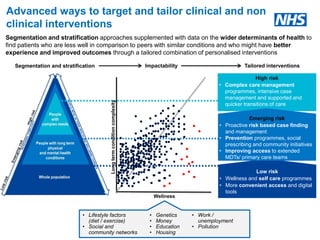
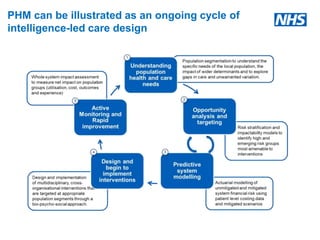
- PHM solutions will help ICSs understand health needs and match NHS services accordingly through data analysis.
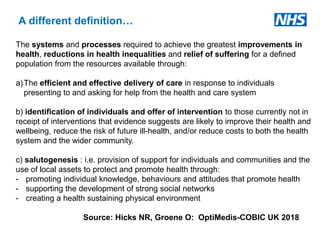
- PHM aims to improve population health through proactive, data-driven care that prevents illness and reduces health inequalities.