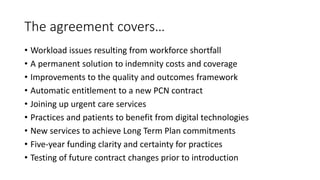
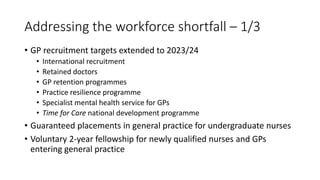
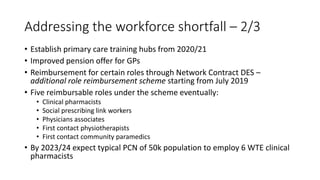
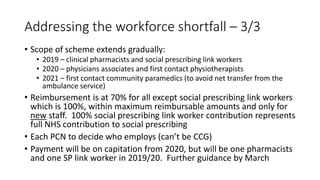
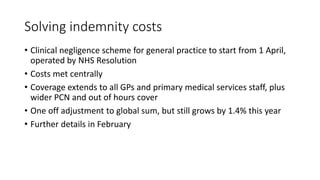
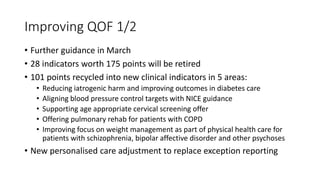
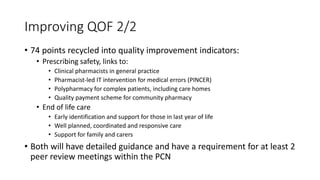
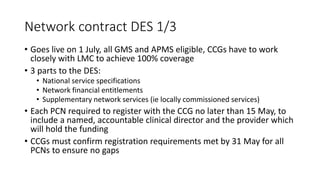
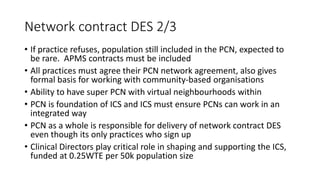
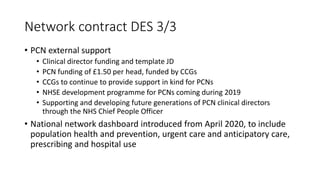
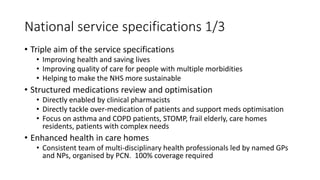
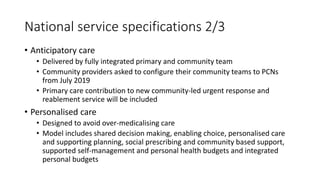
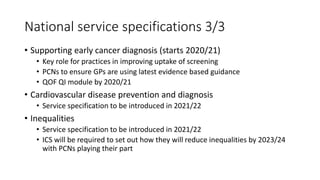
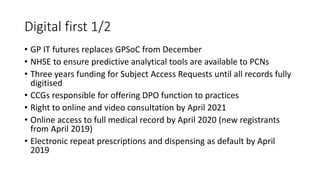
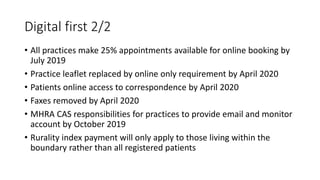
This document summarizes key points of a new 5-year GP contract framework agreement in the UK. It covers addressing workforce shortages through recruitment and retention programs, solving indemnity costs by establishing a new clinical negligence scheme, improving quality measures, establishing primary care networks to integrate services, investing in digital technologies, and guaranteeing funding stability over 5 years. The agreement aims to improve health outcomes, care quality for patients with multiple conditions, and long-term sustainability of the NHS.