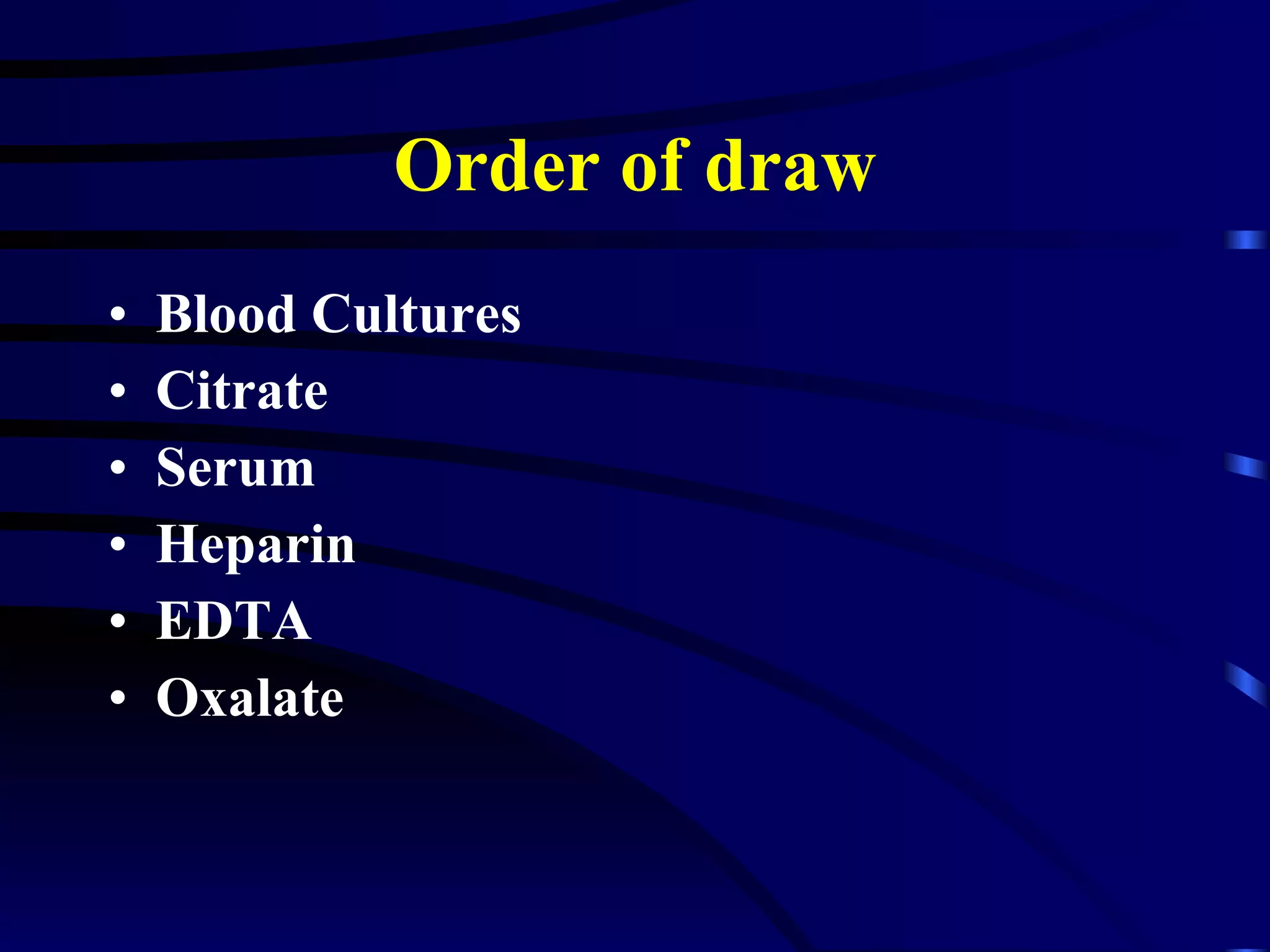
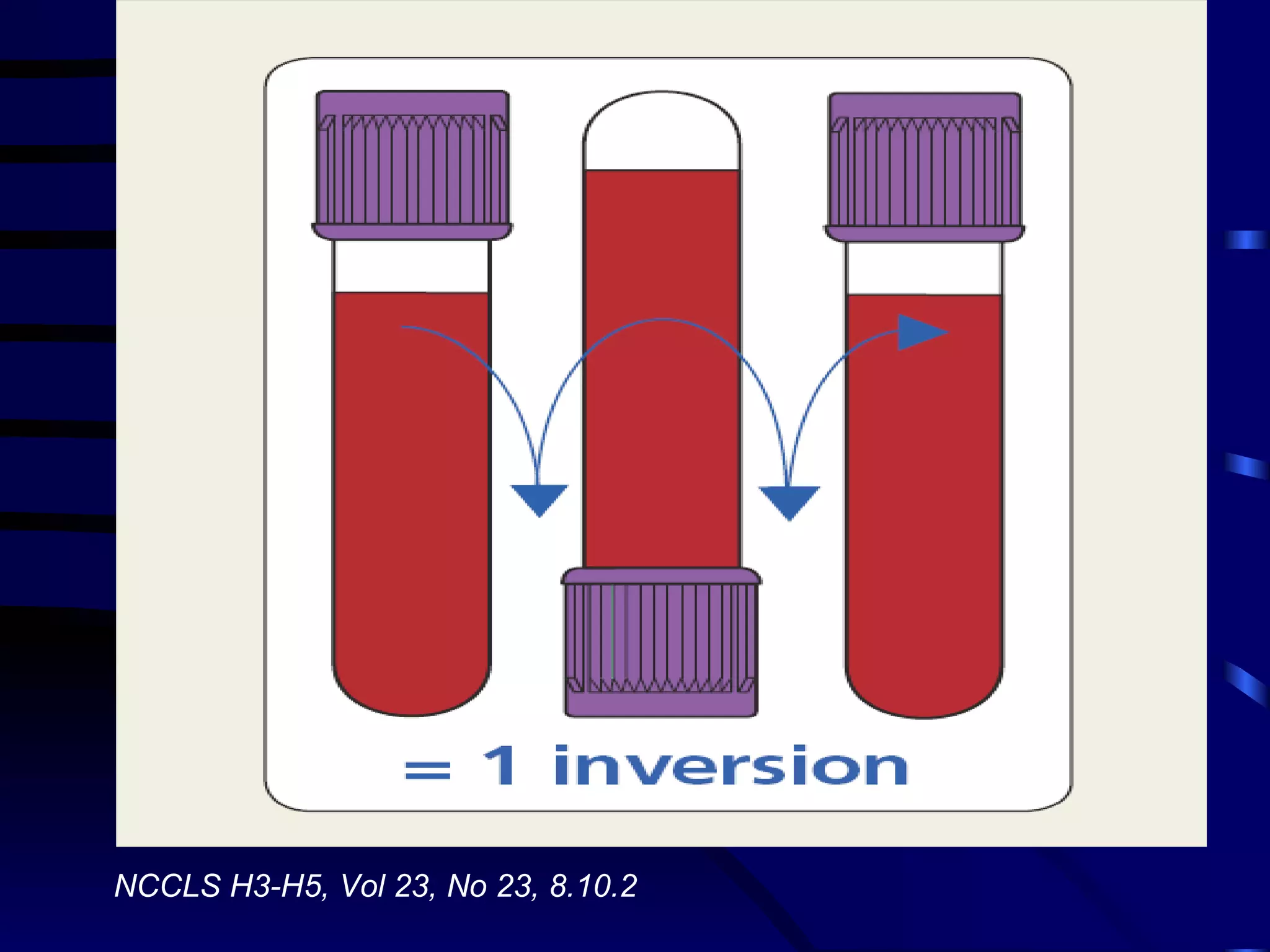
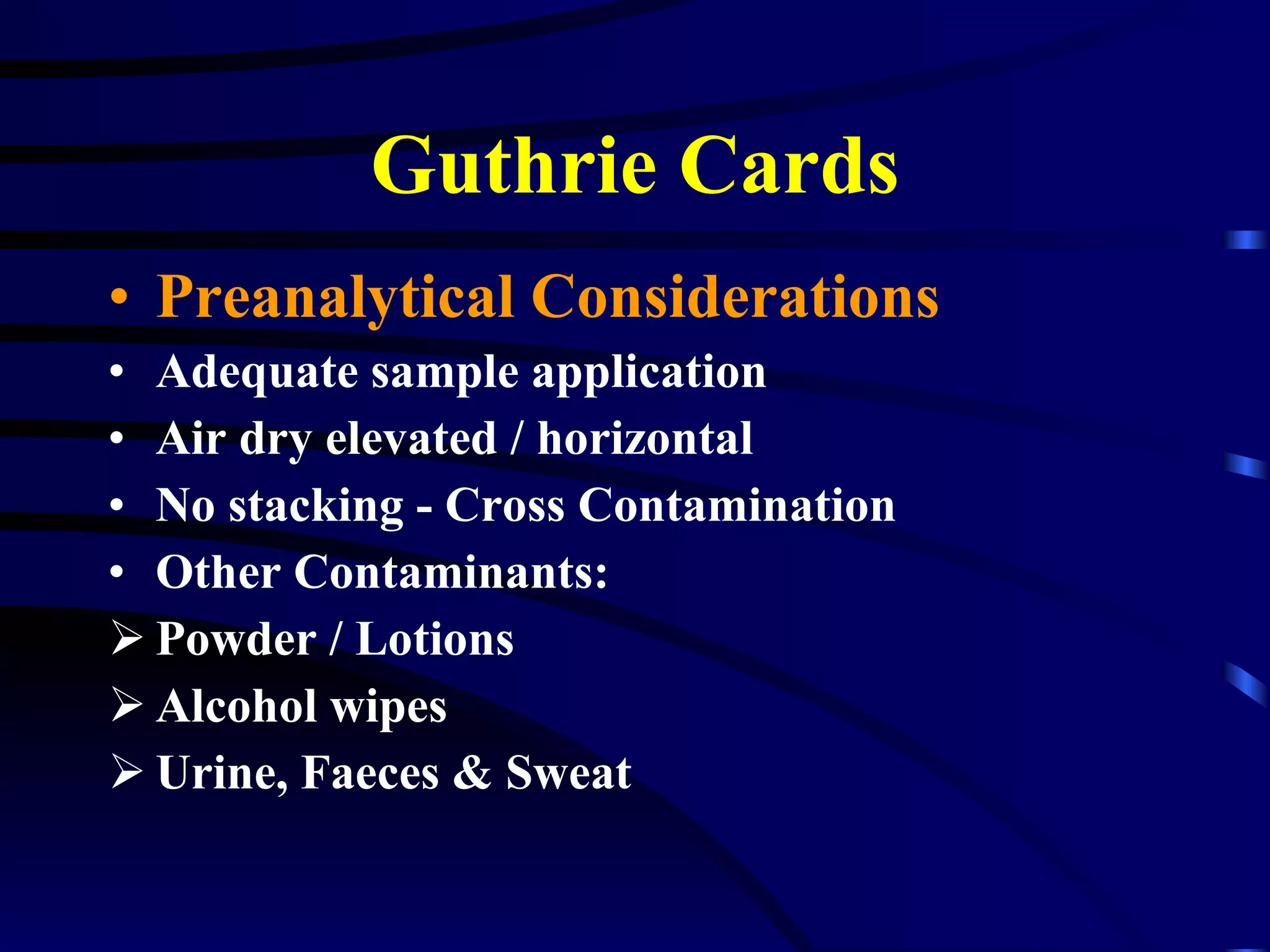
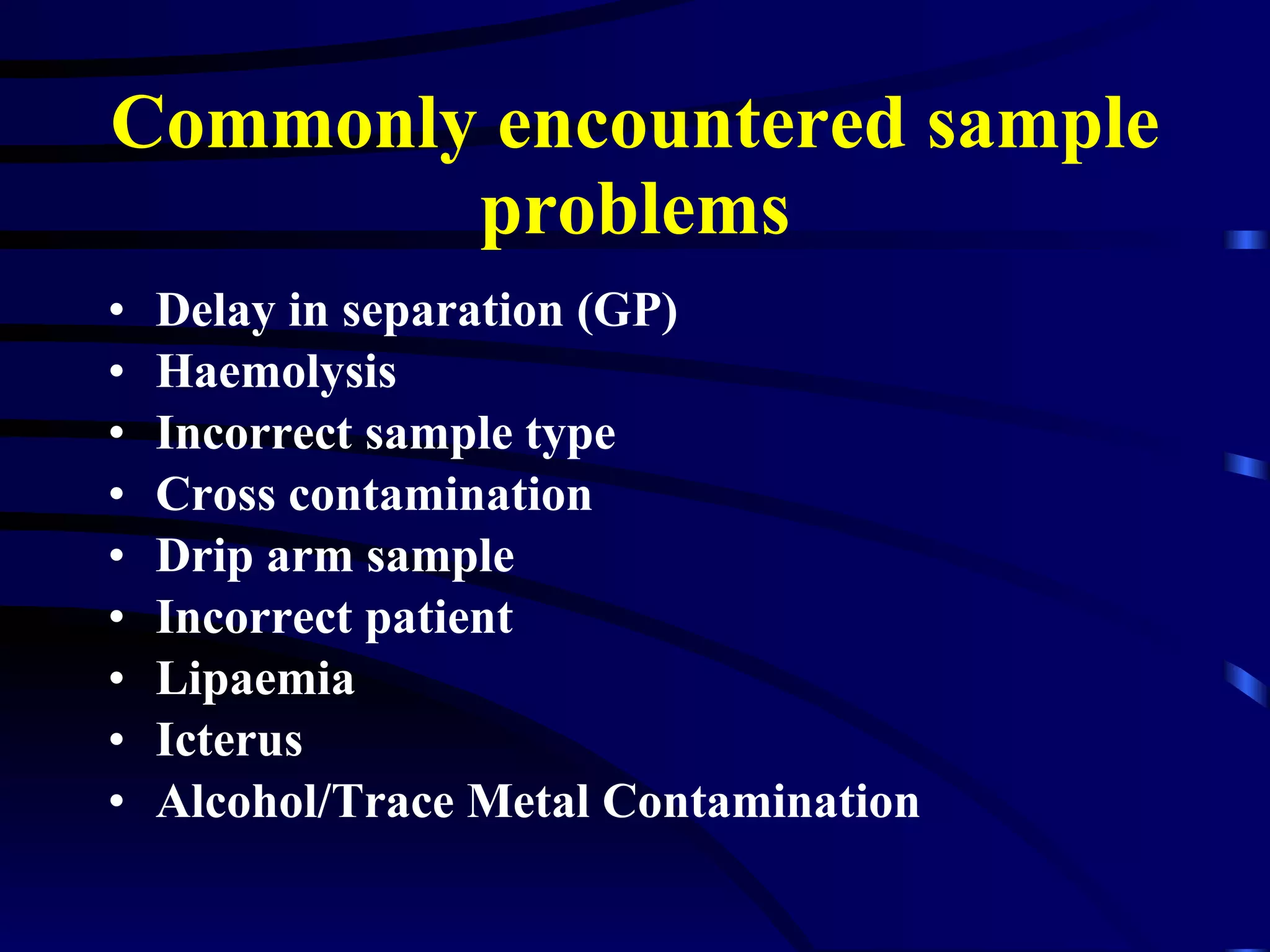
The document provides information about the roles and responsibilities of phlebotomists in a biochemistry laboratory. It discusses key duties like ensuring proper patient identification, sample handling and transport procedures. It also outlines various preanalytical and analytical considerations for sample collection and testing, including different anticoagulants, test types, quality standards and transport methods. The document emphasizes the importance of adherence to protocols and informing the laboratory of any issues that could impact test results.