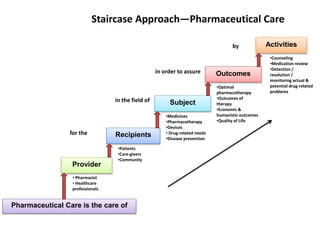
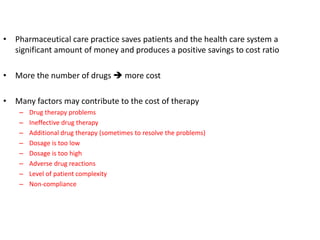
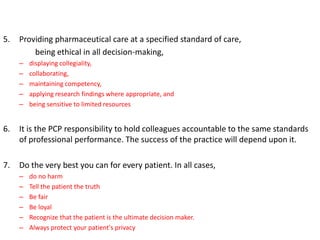
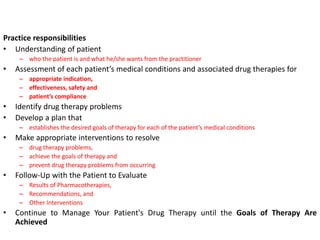
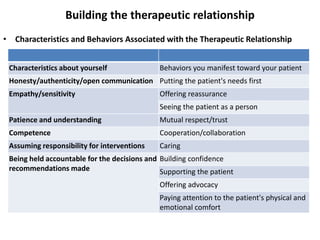
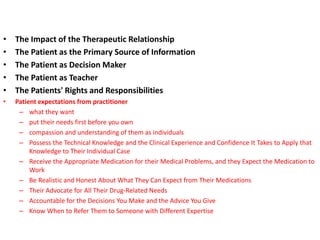
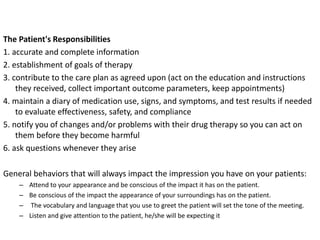
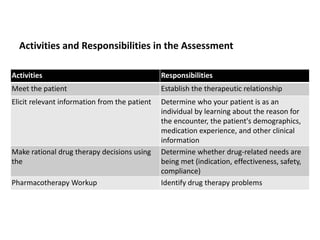
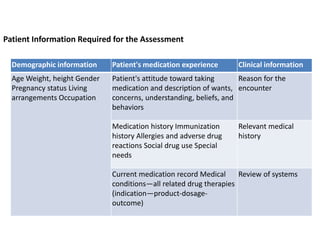
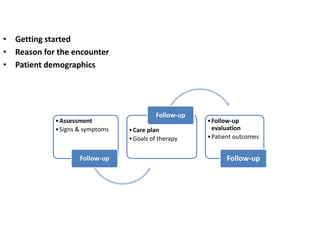
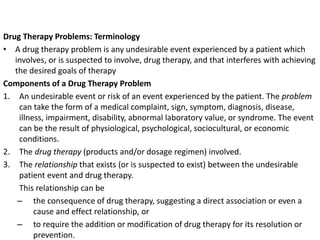
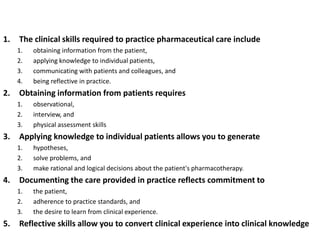
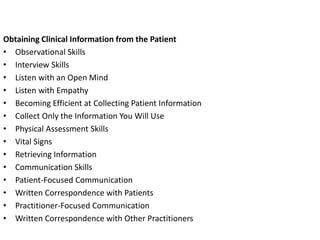
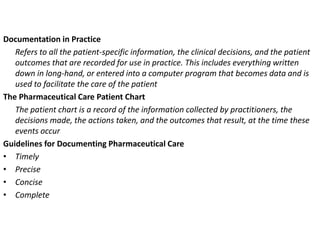
The document provides information on pharmaceutical care including its history and key concepts. It discusses the staircase approach to pharmaceutical care and outlines the practitioner's responsibilities. These include understanding the patient, assessing their medication needs and therapy, identifying any drug-related problems, developing a care plan, and conducting follow-up evaluations. It also covers assessing the patient's medication experience, types of drug therapy problems, and the importance of the therapeutic relationship and patient-centered approach.

![Pharmaceutical Care
• The concept of pharmacy practice took its roots in 1975 as,
“The care that a given patient requires and receives which assures
safe and rational drug usage”
– This concept laid the foundation of “Pharmaceutical Care”
[formally adopted in 1990]
• Pharmaceutical Care concept is the basis of modern days’ picture of
Pharmacy Practice with further room for specialized services (patient-
centered services).
• Pharmaceutical care is a patient-centered practice in which the practitioner
assumes responsibility for a patient's drug-related needs and is held accountable for
this commitment](https://image.slidesharecdn.com/pharmaceuticalcare-1-220829114504-39097dad/85/Pharmaceutical-Care-1-pptx-2-320.jpg)