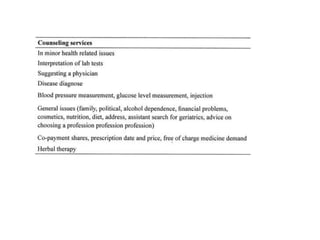
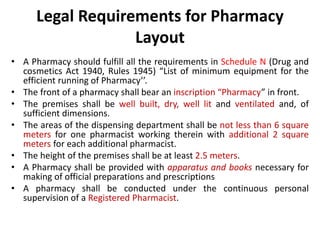
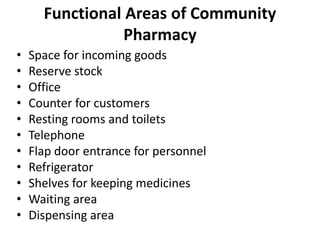
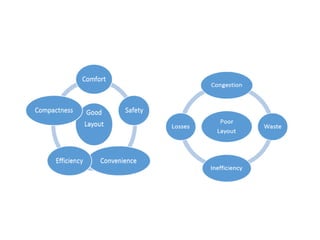
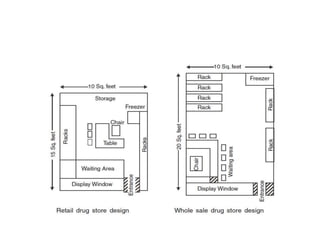
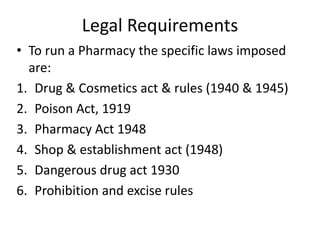
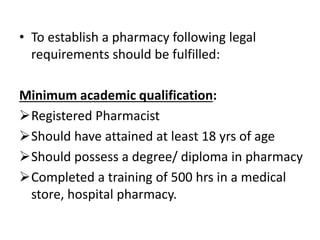
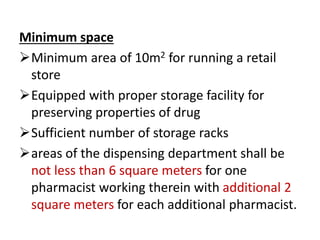
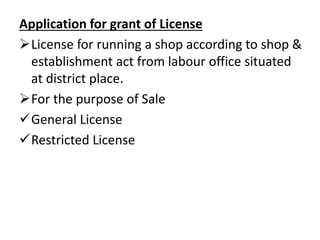
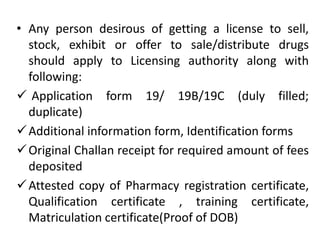
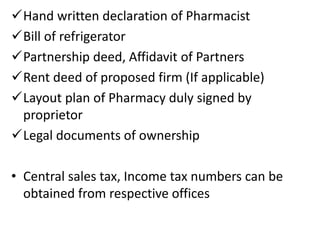
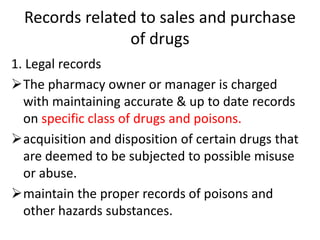
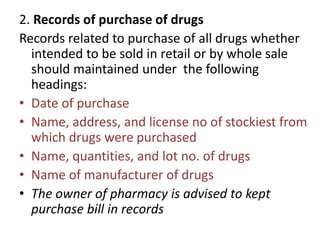
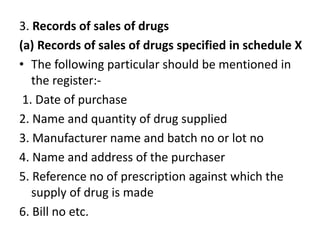
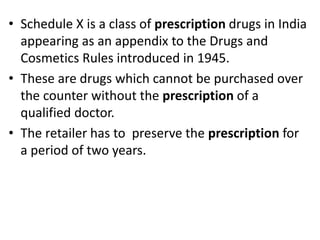
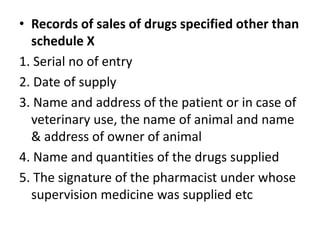
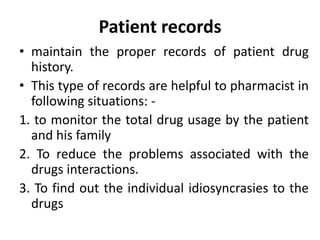
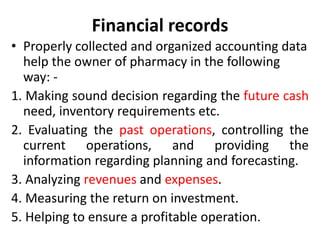
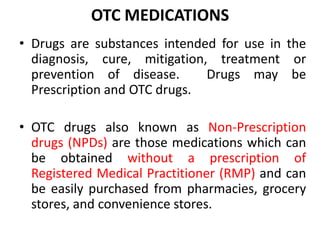
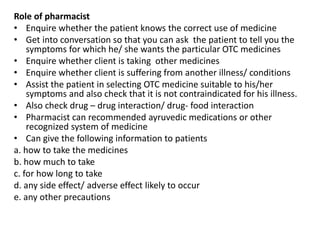
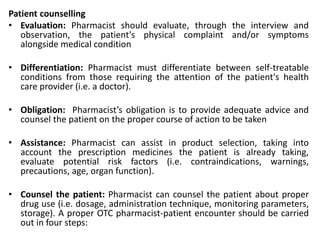
A community pharmacy is a local healthcare facility providing pharmacy services, including the dispensing of medicines, patient counseling, and participation in health promotion programs, operated by registered pharmacists. The scope of community pharmacy is expanding to include patient care, chronic disease management, over-the-counter medication guidance, and medical tourism, while adhering to legal requirements for operation and maintaining various records. Legal obligations include a formal application for licenses, space requirements, record maintenance for drug transactions, and compliance with regulations such as the Drug and Cosmetics Act.