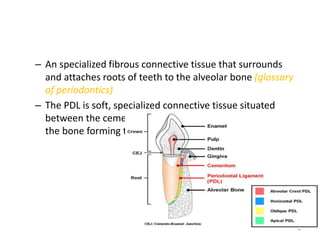
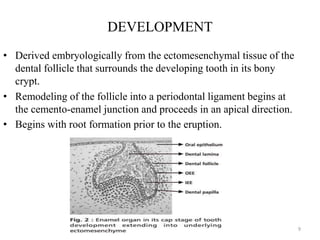
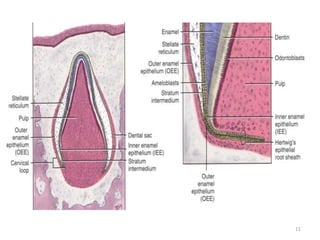
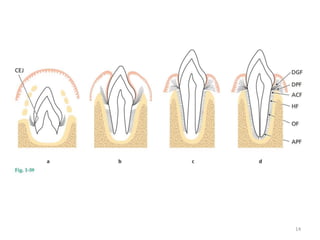
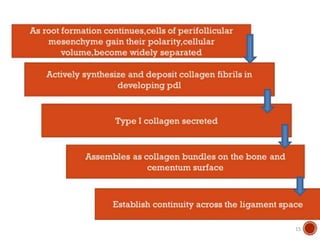
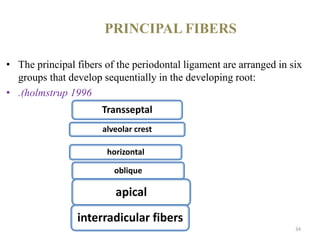
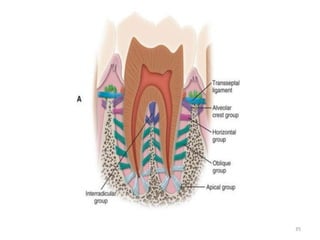
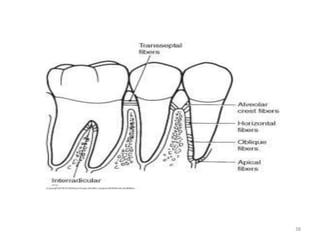
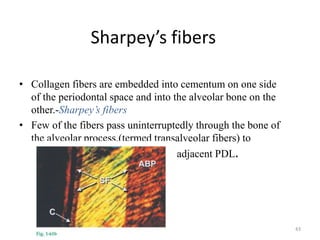
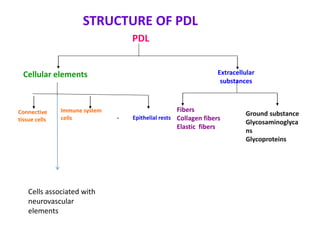
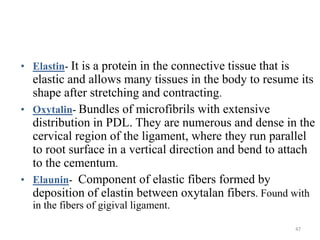
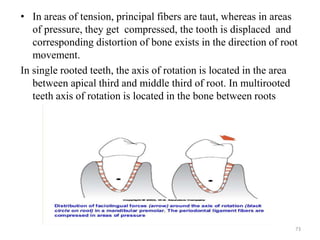
The periodontal ligament is a specialized connective tissue that connects the cementum covering the tooth root to the alveolar bone. It develops from the dental follicle during root formation and eruption. The periodontal ligament is composed primarily of collagen fibers arranged in bundles called principal fibers. These fibers are organized into groups that develop sequentially and provide support, resistance to forces, and sensory functions. The periodontal ligament plays an important role in tooth attachment and is essential for proper occlusion and function.