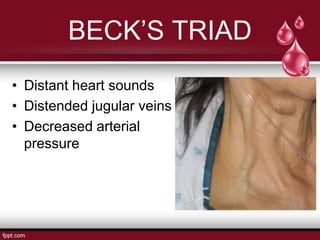
This document discusses cardiac tamponade and pericardial diseases. Cardiac tamponade occurs when fluid accumulates in the pericardial space, increasing pressure and compressing the heart. Common causes include malignancy, idiopathic pericarditis, renal failure, cardiac surgery/trauma, tuberculosis, and hemopericardium. Accumulated fluid under high pressure compresses the cardiac chambers and impairs filling, leading to increased venous pressures and decreased cardiac output. Clinical features include hypotension, elevated jugular venous pressure, muffled heart sounds, and pulsus paradoxus. Management involves relieving symptoms, improving heart function, and saving the patient's life through interventions like diuretics, dig