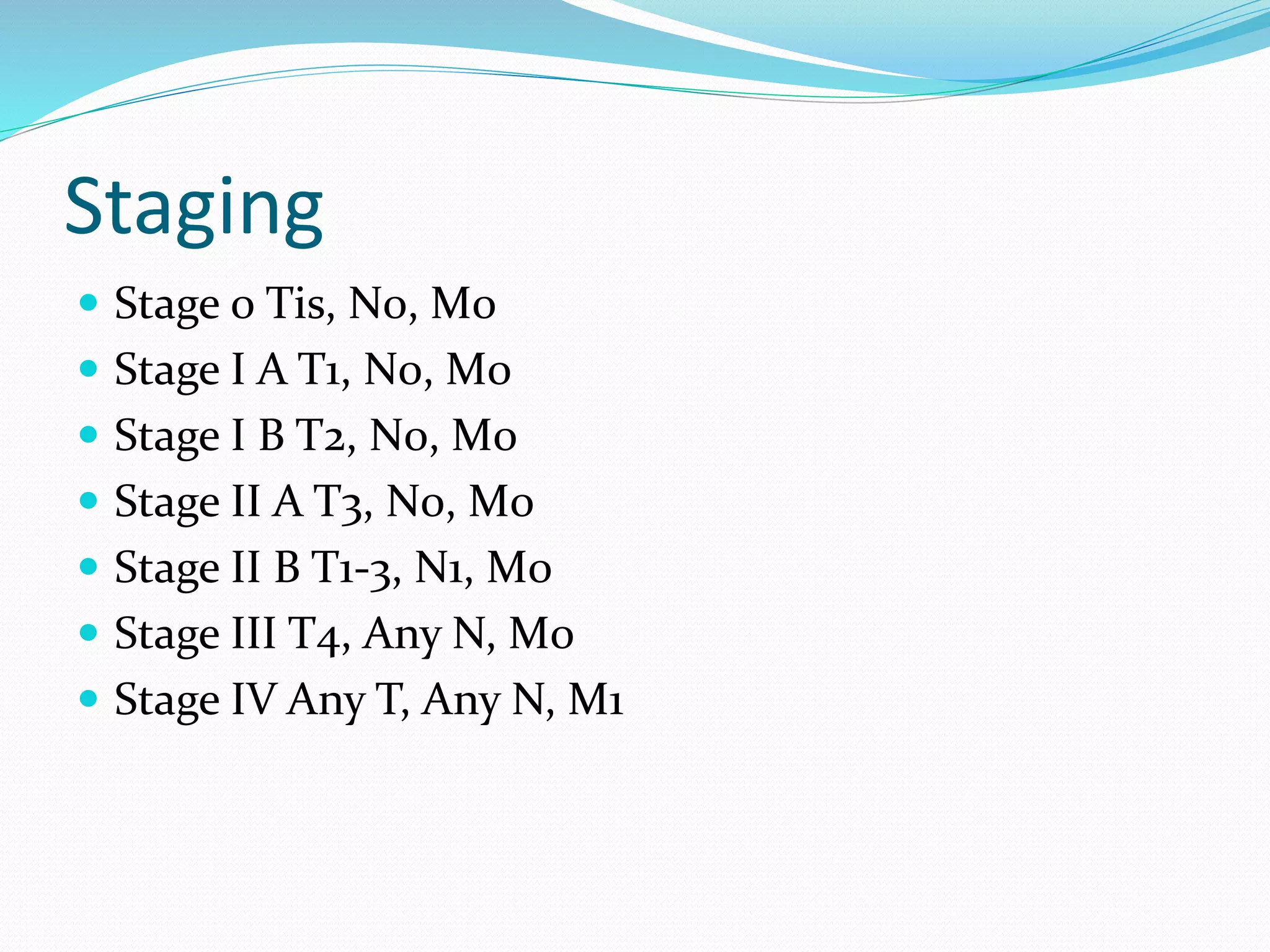
This document discusses periampullary tumors, which arise near the ampulla of Vater. It defines periampullary tumors and lists the components that can be involved, including the bile duct, pancreatic duct, and duodenal mucosa. It then discusses cholangiocarcinoma, a type of bile duct cancer that can present as a periampullary tumor. Risk factors, clinical presentation, diagnosis, staging, treatment and prognosis of periampullary tumors are summarized. Surgical resection offers the best chance of survival, while unresectable tumors may be treated with stenting, radiation or chemotherapy to relieve symptoms.