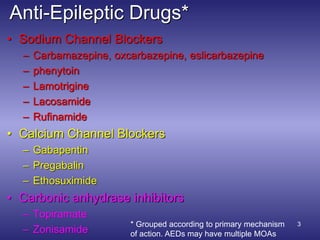
The document provides an overview of anti-epileptic drugs (AEDs), detailing their mechanisms of action, indications, pharmacokinetics, and potential side effects. It discusses various categories of AEDs, including sodium channel blockers, calcium channel blockers, and GABA enhancers, along with specific drugs like carbamazepine, lamotrigine, and sodium valproate. Additionally, the document highlights treatment guidelines and cautions regarding the use of these medications in different seizure types and patient populations.

![10
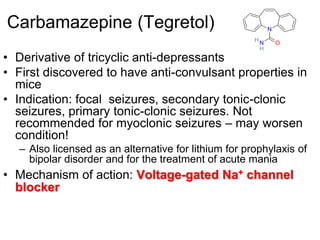
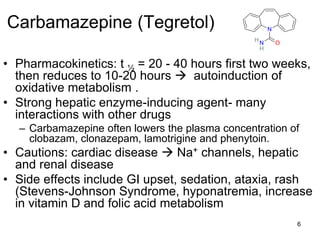
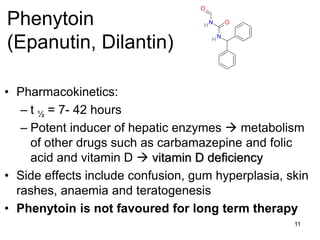
• First discovered to have anti-convulsant properties in
mice
• Indication: Tonic-clonic, focal seizures,
• Mechanism of action: Voltage-gated Na+ channel
blocker
• Pharmacokinetics: low doses exhibit first order
kinetics, saturation kinetics as therapeutic [D]plasma
(10-20 mg/L) is approached dose increments of
equal size disproportional rise in steady state
[D]plasma that varies between individuals
O
N
H
N
O
HPhenytoin
(Epanutin, Dilantin)](https://image.slidesharecdn.com/pepepilepsypart2-190913092416/85/Pep-epilepsy-part-2-10-320.jpg)
![Dr Kelley 20
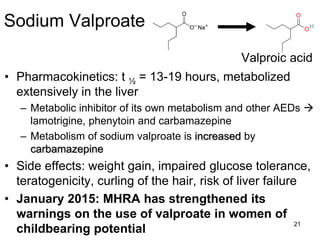
Sodium Valproate
• Mono-carboxylic acid, chemically unrelated to other anti-epileptic drugs
• First discovered to have anti-convulsant properties in mice
• Indication: Effective for all forms of epilepsy, including absence
• Also indicated for bipolar disorder as a mood stabiliser
• Multiple mechanisms of action:
(i) Weak inhibitor of GABA transaminase = [GABA]
(ii) Inhibitor of succinic semialdehyde dehydrogenase = (indirectly)
[GABA]
(iii) May stimulate synthesis of GABA by acting at GAD, = [GABA]
(iv) May decrease GABA reuptake by acting at GAT-1 or GAT-3, =
[GABA]
(v) Weak blocker of voltage-gated Na+ channel blocker
(vi) May block NMDA-mediated responses
O
O
H
Valproic acid](https://image.slidesharecdn.com/pepepilepsypart2-190913092416/85/Pep-epilepsy-part-2-20-320.jpg)