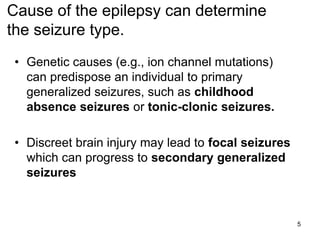
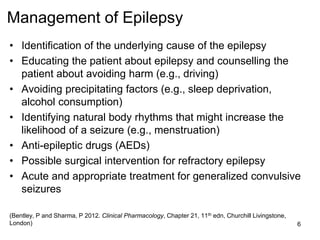
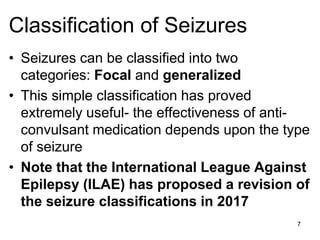
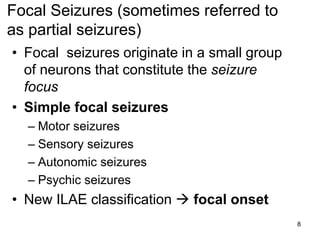
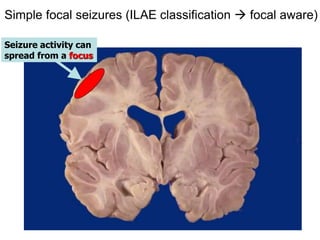
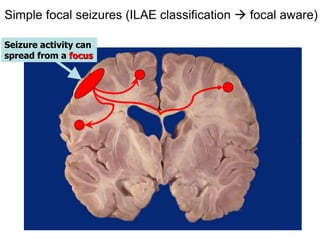
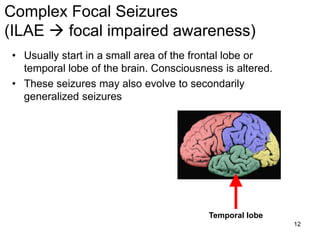
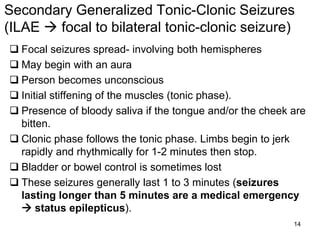
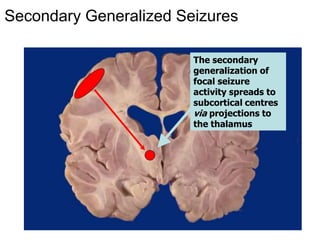
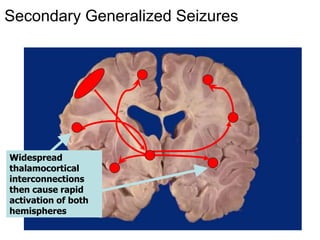
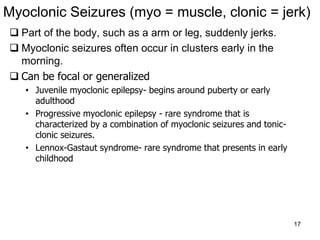
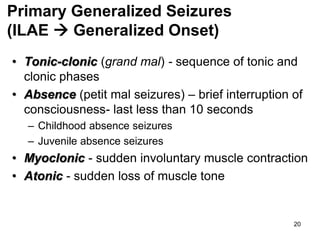
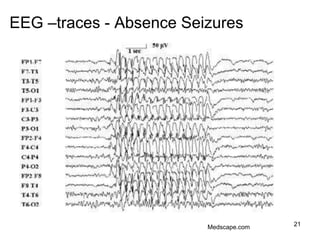
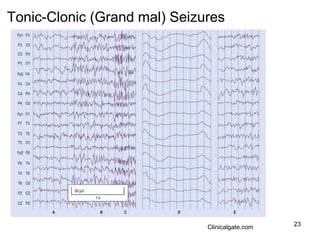
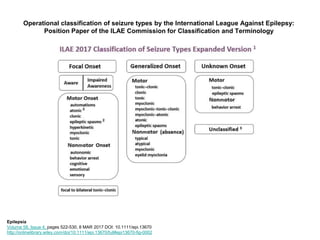
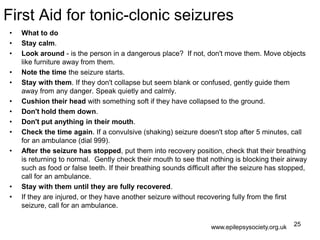
This document provides an overview of epilepsy pharmacotherapy, including classification of seizures and epilepsy. It discusses the pathophysiology and causes of epilepsy, classification of seizure types, management strategies, first aid for seizures, and considerations for pregnancy. Key points covered include the definition of seizures and epilepsy, that up to 1/3 of cases are idiopathic while others are symptomatic, classification of focal and generalized seizures, and first-line treatment involving antiepileptic drugs.