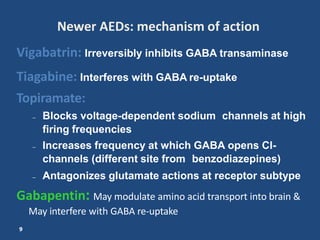
This document discusses antiepileptic drugs, their mechanisms of action, classifications, pharmacokinetics, indications, and adverse effects. It covers older drugs like phenobarbital, phenytoin, carbamazepine, and ethosuximide as well as newer drugs like lamotrigine, gabapentin, vigabatrin, tiagabine, and topiramate. The main mechanisms of action are enhancing GABA transmission, blocking sodium channels, and blocking calcium channels. The drugs are used to treat generalized tonic-clonic, partial, and absence seizures, as well as neuropathic pain and bipolar disorder. Common adverse effects include sedation, dizziness, rash