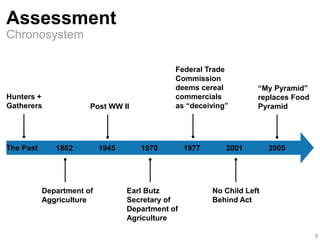
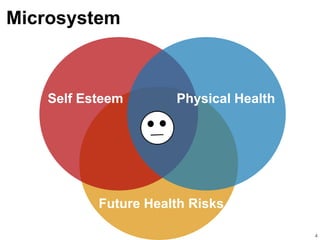
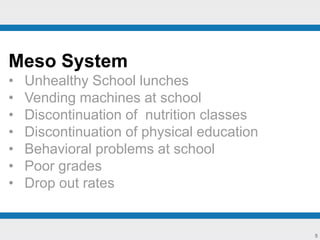
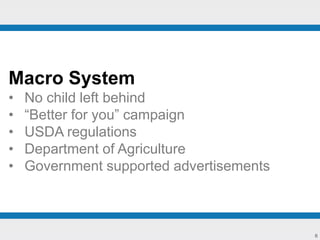
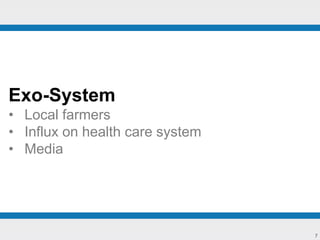
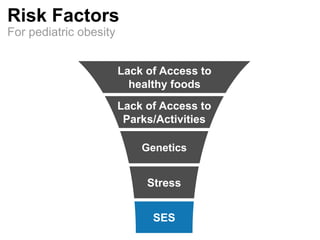
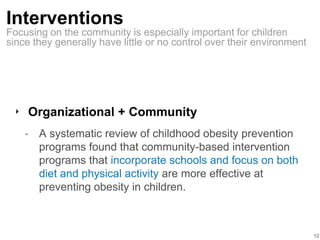
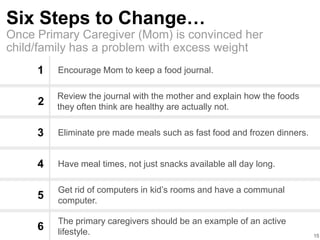
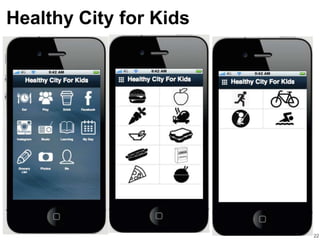
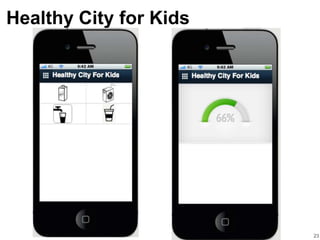
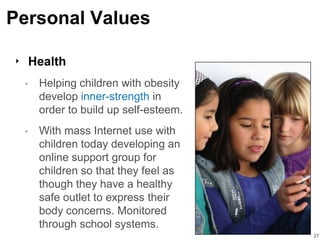
This document discusses pediatric obesity from multiple perspectives. It covers the chronosystem and risk factors for pediatric obesity. Interventions are discussed at various levels, including social, organizational, community, school-based, small group, and individual. Primary, secondary, universal, selective, and indicated prevention and promotion strategies are proposed. Personal, relational, and collective values related to pediatric obesity are also presented, including self-determination, caring, health, respect for diversity, participation, collaboration, community support, and social justice. The overall goal is to empower children and families to adopt healthy lifestyles and prevent pediatric obesity.