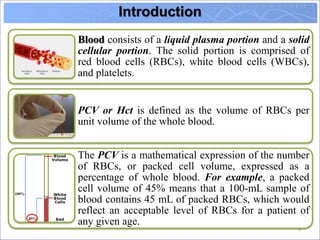
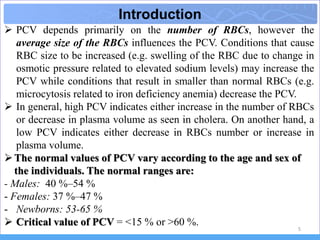
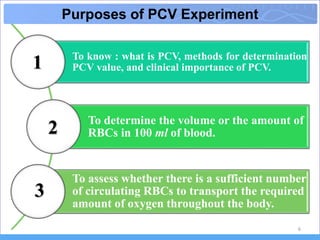
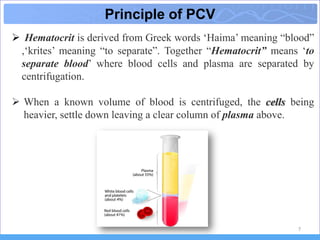
1) The document discusses the determination of packed cell volume (PCV), also known as hematocrit (Hct), which is defined as the volume of red blood cells per unit volume of whole blood.
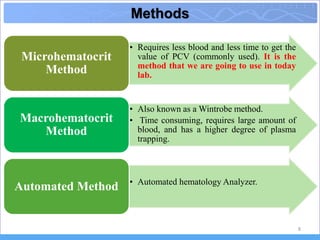
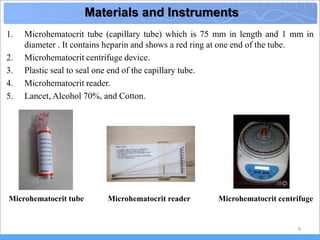
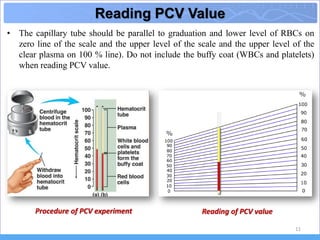
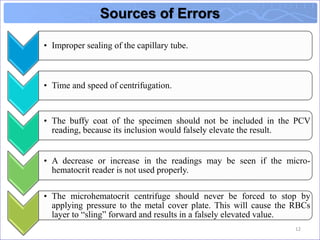
2) It describes the microhematocrit method used in the experiment, involving drawing blood into a capillary tube, sealing it, centrifuging, and reading the PCV value based on the ratio of red blood cell volume to total blood volume.
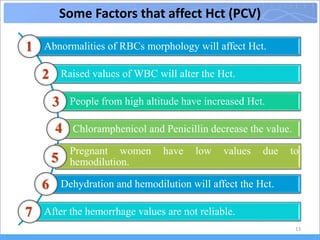
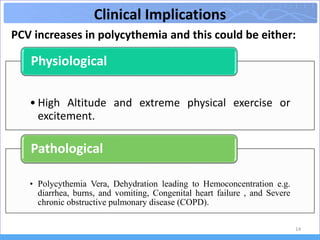
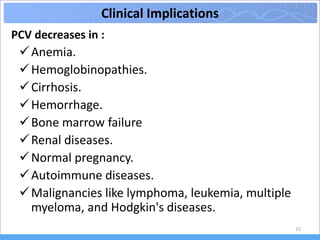
3) Abnormal PCV values can indicate conditions like anemia, dehydration, or polycythemia, while factors like altitude, exercise, and pregnancy can cause physiological changes in PCV.