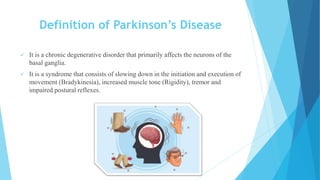
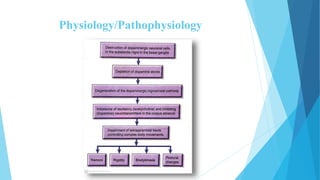
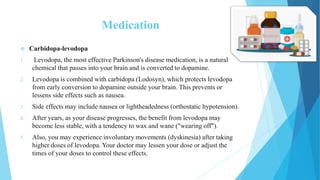
Parkinson's disease is a progressive nervous system disorder that affects movement. It causes tremors, stiffness, and slowing of movement. While the cause is unknown, it involves the loss of dopamine-producing neurons in the brain. Symptoms worsen over time and include tremors, rigid muscles, impaired posture, and speech changes. There is no cure, but medications can improve symptoms by increasing dopamine, and deep brain stimulation surgery may also help in advanced cases. Lifestyle changes such as exercise and a healthy diet can further ease symptoms.